CHAPTER ONE
1.0 INTRODUCTION
Over 100 years ago, all blood had been assumed to be the same and often tragic consequence of blood transfusion were not understood. There were many cases of transfusion reaction due to incompatibility which result to death after transfusion. Effort were made by several researcher to know the possible cause of the blood transfusion reaction (Donnell, 2001)
In 1900 an Austria scientist Karl landstainer discovered the existence of the first known blood group system (ABO). There are over 650 blood group system e.g ABO, Rh, Dusty, kell, Lewis,PI e.t.c ABO and rhesus blood group system are the clinically most important (Donnell, 2001)
The success of human blood transfusion requires compatibility for the two major blood group antigen system, namely ABO and rhesus. The ABO is the most important blood group system in blood transfusion and organ transplantation is defined by two red blood cell antigen A and B, whose presence or absence is determined by three alleles (A, B, O) segregating at a single genetic locus. An unusual feature of this system is the present of serum igM antibodies in healthy adult to whichever antigen (A or B) is absent from individual cells. The presence or absence of Rh antigen on red blood cells is determined by two alleles at another locus Rh. Rh incompatibility between mother and infant may result in ERYTHROBLASTOSIS FETALIS, which can be prevented by passive immunization of the mother with anti-Rh antibodies (RHOGAM). ABO blood grouping is carried out using anti sera to detect the antigen on the surface of the red blood cells. Blood group are permanent inheritance that are passed genetically from one parent or both to an offspring or progeny base on mendelian law of inheritance. It is important for one to know his or her blood group to prevent transfusion reaction, haemolytic disease of the born and others complication. (Laffan, 2001).
1.1 JUSTIFICATION
Blood grouping is an important investigation carried out in the laboratory to prevent blood incompatibility that result to the effect on maternal-fetal interaction and blood transfusion reaction, due to incompatibility testing that leads to death after transfusion, this shows great need for this research on the importance of ABO and Rhesus blood grouping effect to the community.
1.2 AIMS AND OBJECTIVE
- To enlight the audient on Rh factor and importance in maternal-fetal interaction.
- To know more on blood incompatibility.
- To educate on the importance of ABO and Rhesus blood grouping.
PTER TWO
2.0 HISTORY
ABO blood group system was discovered in 1900 by Austrian scientist, Karl Landstainer, after he mixed the red cells of a number of individual with the serum of the others in the experimental group. Landstainer Karl observed that some combinations resulted in agglutination where as others did not. He found that he could classify the agglutination patterns into three groups which he designated A, B and O. He showed that those in group A possessed and antigen (A antigen) On their red cell which reacted with antibodies (anti-A) in the serum of those in group B or O. similarly, those in group B possessed B antigen on their red cells which reacted with antibodies (anti B) in the serum of those in group A or O (Landstainer, 1900).
The red cells of those in group O were not agglutinated by either A or B serum. A few years later, the group identified another group which showed both A and B red cells antigens (Landstainer, 1900). After this discovery, the ABO blood group system was used to explain the majority of incompatible blood transfusion.
The Rhesus blood group is one of the most complex blood group known in humans from its discovery 60 years ago where it was named (in error) after the rhesus monkey, it has become second in importance only to the ABO blood group in the field of transfusion medicine (Westhoff, 2004) it has remained of primarily importance in obstetrics being the main cause of hemolytic disease of the new born (HDN) (Westhoff, 2004).
The significance of the Rh blood group is related to the fact that the Rh antigens are highly immunogenic. In the case of the D antigen, individual who do not produce the D antigen will produce antigen-D. if they encounter the D antigen on transfused RBSc (Causing a hemolytic transfusion reaction, HTR) or on fetal RBCs (causing HDN) (Wagner, 2003). for this reason, the Rh status is routinely determined in blood donors, transfusion recipients and in mothers-to-be.
ABO Blood Groups
The ABO group are defined by the presence of two alternative antigens on red blood cells, determined by three alternative alleles at a single genetic locus (Reid, 2004) two basic rules governing this system are;
- The blood “type” is defined by the presence of two red blood cell antigen “A” and “B” RBCs of type A have the A antigen on their surface, those of type B have antigen B, type AB red cells have both antigens, while type O cells bears neither antigen.
- “Natural” antibodies called isoagglutins exist in an individual serum. Directed against whichever of the A and B antigens is not present on that persons red cells (Francis, 2004).
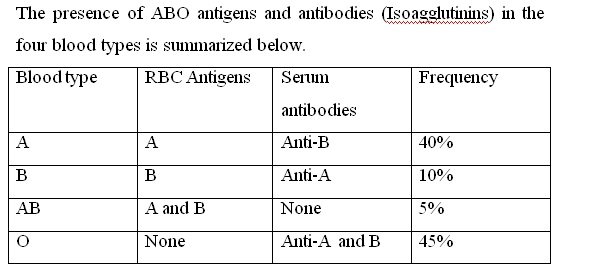
The converse presence of Anti-A and anti-B agglutinins in serum means that ABO grouping can be performed on both red cells and serum. This act as a double check to ensure that the correct ABO group has been determined and should always be performed as part of a compatibility test prior to transfusion.
2.2 GENETICS OF ABO
The presence of A and B carbohydrates in our tissue is determine by three alleles at a single genetic locus one allele encode an enzymes which produces the A substance, another the B substance and when both of these alleles are present in a heterozygote both carbohydrates are made. The third allele O behaves essentially as a “null” allele. Producing neither A nor B substance. Thus, while the ABO system yields only four blood types (Phenotypes). There are six possible genotype (Blackwells, 2002)
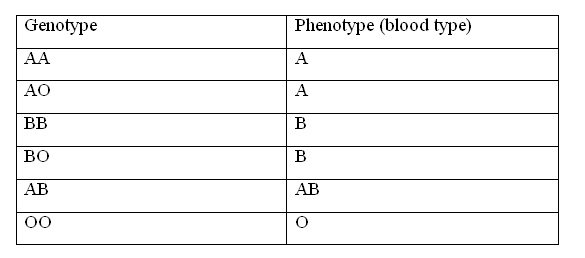
Only a single genotype can produce the phenotype AB namely the heterozygous state AB likewise, type O individual must be homozygous OO. However, type A or type B individual can be either homozygous or heterozygous. The O allele being effectively recessive since it does not contribute either of the two antigen (Bird, 1990).
The inheritance of ABO blood group follow simple mendelian rules for instance a homozygous type A mother and a type AB father can yield only two kinds of offspring type A (Genotype AA) or type AB (Genotype AB). A heterozygous type A and a heterozygous B, on the other hand can yield four genotypes with four corresponding phenotypes.
2.3 ABO SUB GROUPS
The A blood type contain about 20 sub group of which A and B2 are the most common (Over 99%). A1 make up about 80% of all A types blood with A2 making up almost all the rest (Seltsam A 2003).
These two sub group are not always interchangeable as far as transfusion is concerned, as some A2 individual produce antibodies against the A1 antigen, complication can sometimes arise in rare cases when typing the blood (Seltsam A, 2003)
Distribution Worldwide
The distribution of the four ABO blood types A, B, AB and O, varies in population throughout the world. It is determined by the frequency of the three alleles of the ABO gene in different population. Blood types O is the most common worldwide, followed by group A. Group B is less common and group AB is the least common.
Function of the A and B antigen and Rh
The function of ABO blood group antigen are not known. Individual who lack the A and B antigens are thought to play a role in maintaining the integrity of the RBC membrane-RBCs which lack Rh antigen have an abnormal shape.
2.4 DISEASE ASSOCIATED WITH ABO BLOOD GROUP ANTIGEN
No disease are known to result from the lack of expression of ABO blood group antigens, but the susceptibility to a number of disease has been linked with a person’s ABO phenotype such correlation remain controversial and include the observation that gastric cancer appear to be more common in Group A individual (Bird, 1990), whereas gastric and duodenal were occur more often in group O individual (Laffan, 2001)
Blood Typing and Cross-Matching
The presence of these antigens and antibodies can be readily detected by the agglutination reaction, mixing type A plasma (Which contain anti-B antibodies) with type B red cells, for instance. Result in agglutination of the red cells which can easily observe. The blood type of any given individual can be determined. Carrying out the agglutination reaction with a set of standard antibody containing sera. Before a blood transfusion is given, in addition to choosing donor blood only of the same ABO type, direct cross matching of donor and recipients serum to guarantee that the original typing of donor and recipient was correct and to detect any possible unexpected agglutination reaction (Williamson, 1999).
The primary cause of ABO mismatches transfusion reactions from destruction of donor red cells by the recipients antibodies and recipients cells is of less importance, since the small amount of antibody contained in the transfusion is generally diluted to harmless level in the recipients. As a result, a type O individual (whose red cells bear wither antigen) is referred to as Universal donor since his blood can fairly safety be given to a recipient with any ABO type, conversely a person of blood type ABO has been called a Universal recipient since his blood will contain no AB antibodies to damage any transfused red cells.
2.5 SELECTING BLOOD FOR TRANSFUSION
The first choice of blood for a patient should be blood of the same ABO group and Rh group as the patient. Avoid transfusion group O blood to those who are not group O, particularly when needing to use whole blood because group O blood can contain dangerous Immune anti A and anti B haemolysin. The risk is reduce when using concentrated red cells. When no blood or insufficient blood of the sauce ABO group as the patient is available, select blood as shown in the following chart;
Group of patient Choice of blood
1st 2nd 3rd 4th
Group A GPA GPO - -
Group B GPB GPO - -
Group AB GPAB GPA GPB GPO
Group O GPO
2.6 THE IMPORTANCE OF BLOOD GROUPING
The blood grouping is very important when it comes to having a blood transfusion (Haemolytic transfusion reaction). If blood is given to a patient that has a blood type that is incompatible with the blood type of the blood that the patient receives, it can cause intravenous clumping in the patient’s blood which can be fatal. The patient body can start producing antibodies that attack the antigens on the blood cells in the blood that was given to the patient. For example a patient who is blood group B has naturally occurring Anti-A antibodies in the blood if this (blood group B) patient receive blood group A blood, the anti- A antibodies in the blood of the patient who is blood group A has naturally occurring anti bodies anti B in the blood. Blood group O can be given to any other blood group since there are no naturally occurring antibodies in the blood of someone who is blood group O (Sazama, 1990).
Considering that a person can be either blood group A, B, AB or O and is either Rh group positive (+) or negative (-) this means that a person can be one of eight blood groups: A+ A- B+ B- AB+ AB- O+, O- people who are blood group RhD positive or negative blood but people with RhD negative blood can only receive Rh negative blood.
HEMOLYTIC DISEASE OF THE NEW BORN
In child bearing, the Rh blood group system is the major cause of hemolytic disease of the newborn (HDN) that start in the uterus and cause jaundice, Anemia and hepatosphenomegaly mental retardation and still birth if a woman who is Rh D negative is married to a man who is Rh D positive fetus and fetus is at high risk of (HDN). If some of the fetus blood posses into the mothers blood circulation during child birth (Feto maternal hemorrhage) the mother will be sensitized and produce antibodies against fatal antigen (having recognized the fetus blood as foreign). The first fetus is usually not at risk since the fetal red blood cells do not enter the mothers circulation until the time of delivery (Kayode 2010) when next the women is pregnant with a second Rh “D” positive fetus the Mothers red cell (19G anti-D) crosses the placenta into the blood circulation of the fetus and destroys the fetal red cells. This could lead to miscarriage, still birth or jaundice with severe hemolytic anemia.
Another importance of knowing your blood group is to make authentic reliable whenever biomedical information is required in this category.
Remedy
• By knowing your blood group.
• By giving injectable medication IgG anti-D (Rhogam) within 72 hours of giving birth.
• By avoiding transfusion of RhD positive to RhD negative.
2.7 TECHNIQUE FOR ABO BLOOD GROUP
The safe transfusion of a patient depends on the correct ABO grouping of donors and recipients.
ABO blood group is classified into two groups.
i. Cell grouping (tile method)
ii. Serum group (tube method)
Cell Grouping
Principle; Based on antigen/antibody reaction
Material; tile, Pasteur pipette, normal saline. Anti-A, Anti-AB, A cells, B cells, O cells, cotton wool patient blood cells.
Tile method for cell grouping
- Divide and mark a white tile into four.
- Pipette into each division as follows.
a. 1 volume of anti A serum
1 volume of 20-30% patient’s red cells
b. 1 volume of Anti B serum
1 volume of 20-30% patient’s red cells
c. 1 volume of anti AB serum
1 volume of 20-30% patient’s red cells
d. 1 volume of patients serum
1 volume of 20-30% patient’s red cells - Mix the content of each division using a small clean piece of applicator stick for each.
- Tiling gently the tile from side to side, examine microscopically for agglutination after 3 minutes, record the result in the ABO grouping book.
Precaution - During ABO blood grouping ensure that sample to be grouped are properly labeled (both the form and sample)
- Avoid using lyses blood for ABO blood group.
- Avoid using expired anti-sera.
- Freshly prepared pooled red cells should be used.
Techniques For Cross Match
There are two methods used in compatibility testing, they are; - Emergency compatibility.
- Full compatibility testing.
Emergency Compatibility Testing
In emergencies in which immediate red cell support is required, there may not be time for full compatibility testing.
Basically emergency compatibility testing can be classified based on the time involved in the cross match there are two basic groups; - 30 minutes cross match.
- 15 minutes or less cross match.
- Emergency cross match (30 minutes) this consist of two test only.
a. Moist chamber slide at room temperature.
b. Indirect anti-human globulin (AHG) at 370C
a. Moist chamber slide at room temperature; one drop of the patients serum is mixed with one drop of 2% suspension of donors washed red cells on a carefully labeled slide. The tests are allowed to stand in the moist chamber for 10-15 minutes and the result read, all negative reaction being checked microscopically.
b. Indirect AHG at 370C
The test is performed with the patient’s serum against red cells from each proposed donor and the patient’s own cells which serum as control, the indirect AHG is set up in the usual way except that the incubation time reduced to a minimum of 20 minutes after which the result is read macroscopically and microscopically.
Emergency compatibility testing for 15 minutes or less.
This consist of 3 test only;
• Low spinning technique.
• Less (low ionic strength saline)
• Enzyme technique.
Low spinning technique
• The donor’s blood is washed with normal saline.
• They washed donor red cell is mixed with patient serum (equal volume) spun at 150-200g for 5 minutes.
• After centrifugation, albumin is added to the tube and incubated for 5 at 370C
• Spin at same speed for 5 minutes.
• Examine microscopically and macroscopically for agglutination.
CHAPTER THREE
3.0 CONCLUSION
ABO blood group and cross match are very important in blood banking in order to avoid ABO and Rh incompatibility. It is important that cell and serum grouping is performed on all sample as it is a double check.
ABO and Rh grouping are the first test done on blood when transfusion is required before blood from a donor and the recipient are cross matched, both ABO and Rh blood group are typed. ABO incompatibilities are the major cause of fetal transfusion reactions. ABO compatibility is also important for organ transplant.
3.1 RECOMMENDATIONS
I therefore recommended that;
- Blood grouping should be conducted before transfusion take place.
- Expectant mothers should promptly attend ANC clinic. This will help to know those with Rh D negative
- It is also important for an individual to know this or her blood type.
- The government should provide free blood grouping testing for couples before marriage in order to reduce the cases of Rh incompatibility in Nigeria.
References
- Avent ND, Reid ME (2000). The Rh blood group system: A review, blood. 95:375 (Pubmed:106274381)
- Boral LI, Henry JB (1977). The type and screen: A safe alternative and supplement in selecting surgical procedures. Transfusion 17:163.
- Daniel G (2002). Human blood group second Ed. Blackwell science.
- Landsteine K (1900) 2 ur Kemitmis der anti-fermentation. Lytischen und agglutimerenden wirkungen des Blutserums under lymphe “Zentrailblant Bakteriologie 27:357-62
- O’Donnell J, Laffan MA (2001). The relationship between ABO histo-blood grouping factor vill and von willeberd factor, Transfus Med 11(4) : 3432189
- Reid ME, Bird GW (1990). Association between human red cell blood group antigen and disease. Transfus med rev. 4:47-55 (Pubmed:2134616)
- Reid ME, LOMas-Francis C (2004). The blood group antigen Facts Book seconded. New York Elsevier Academic press.
- Rumsey DH, Cleseike DJ (2001) New Protocols in serology testing. A review of technique to meet todays challenges 17:131.
- Sazama K (1990) Report of 355 transfussion associated deaths: 1976 through 1985. Transfusion. 30:583-90 (Pubmed 2402771)
- Standard For blood banks and transfusion service (1999). 19th ed, America Association of blood banks. Bethesda.
- Urbaniak SJ, Greiss MA (2000). RhD haemolytic disease of the fetus and the newborn. Blood Rev: 14:44-61(Pubmed:10-805260)
- Wagner FF, Kasuke D, Kerowgan M, Flagel WA (1995). Frequencies of blood groups ABO. Rhesus D category U, Kell and of clinically relevant high frequency antigen in South Western Germany infusions Transfussion Med.22:285-90 (Pubmed).
Welcome to Steem. Do read A thumb rule for steemit minnows - 50:100:200:25 for starter tips.
Also get to know more about Steem reading the Steem Blue Paper and share your feedback on our Steem Blue Paper Awareness Initiative
All the Best!!!
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
welcome!
fav here :)
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit