I want to be in 2015. I had to take care of an acquaintance who was admitted to a university hospital. As usual, I had an experience where I was sanctioned for being unable to enter a hospital room without a guardian access card. The MERS infection changed the culture of hospital use.
Although not as much as the current coronavirus infection, the fear of MERS infection at the time was also threatening. While evaluating the MERS outbreak, we mentioned our visiting culture and hospital shopping culture as factors that instigated the spread of MERS infection. The family takes care of the critically ill care, and the sick can freely go to this hospital and receive treatment. At the same time, the following plans were suggested.
In order to improve the medical system vulnerable to infection revealed in the MERS outbreak, strengthen hospital infection management, expand comprehensive nursing promptly, resolve overcrowding in emergency rooms, suppress'hospital shopping', and strengthen primary care at the same time. Hospital use culture should be improved.
After the MERS outbreak, infection control offices in each hospital were strengthened, and according to the guidelines, nurses were also forced to put trash bins in the patient treatment room on the right or left side of the door regardless of work efficiency. In addition, restrictions on visiting hospitals were strengthened, and glass doors were installed at the entrances of each ward.
In addition, about 40% of MERS-infected patients are the patient's family or caregiver, and it was evaluated that private care by the patient's family and caregiver increases the patient's risk of hospital infection. Thus, in order to manage hospital infections, a comprehensive nursing service was started in which inpatients are nursed by nurses rather than guardians. All were projects requiring state budget.
Hospital infections are spread to the patient's surrounding environment by infected blood, mucous membranes, damaged skin, and various body fluids, or through various routes such as person-to-person contact. have. In particular, nurses account for the largest number of medical staff in hospitals and have many opportunities to directly contact patients, so the role of nurses in hospital infection management is very important.
Most of the causative bacteria that cause nosocomial infection are Methicillin-Resistant Staphylococcus Aureus (MRSA) and Vancomycin-Resistant Enterococci (VRE). In Korea, hospital infections caused by MRSA and VRE have steadily increased, and MRSA accounts for 70-80% of all Staphylococcus Aureus strains in general hospitals and university hospitals.
Hospital infections have three times longer periods of use of the quarantine room for infected patients than those with legal infectious diseases, and the use of the quarantine room for infection control also results in significant economic losses due to the high-level room charges. In the case of medical institutions, hospital revenues are also reduced due to lower bed turnover.
Eventually, nosocomial infections not only threaten the life of patients, but also cause economic losses to individuals, medical institutions, and countries alike.
There was an interesting content that lowered the hospital infection rate by investigating the coronavirus that is spreading worldwide recently. In the intensive care unit, patients in a place treated with copper alloy on the surface of items frequently touched by medical staff had less than 50% of hospital infections than those in the intensive care unit who placed general hospital items. It doesn't cost much, and only copper is attached to the surface of the item. Looking at this study, I thought that it would be possible to efficiently manage hospital cross-infection that can occur between medical staff or patients and medical staff.
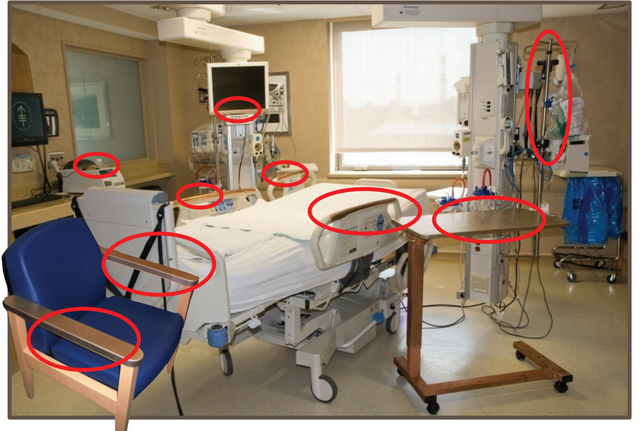
The study conducted 8 items with copper alloy surface treatment in three hospital intensive care units in the United States (bed railing, bed table, intravenous injection stand, guardian chair armrest, nurse call bell, computer mouse, computer monitor bezel, laptop wrist rest) This study compared the incidence of nosocomial infections in intensive care unit patients who placed copper alloy-treated articles on the surface and those who did not. In this study, it should be noted that it is methicillin-resistant Staphylococcus aureus (MRSA) or vancomycin-resistant Enterococcus (VRE), which accounts for 70-80% of Korean pathogenic infectious bacteria. The research team found that copper's persistent antibacterial effect lowered the rate of hospital infection.
In the mid-19th century, copper was a metal used for wound healing and general hygiene. In Britain, France, and the United States, where copper's antibacterial effect was confirmed, there were places where copper alloys or copper materials were used in hospital rooms. In particular, there have been reports that copper kills the coronavirus, and the Korean MediFiber company has developed a virus buster copper filter that kills the coronavirus. How about applying the hospital equipment used in the above study to the hospital environment in Korea? Compared to the economic losses that patients and hospitals have to bear, I think that hospital infections can be managed efficiently without incurring large costs.
Recently, several hospitals in Korea have reported confirmed patients infected with coronavirus. There is no reason not to use hospital virus buster copper filters for the safety of patients and staff.