In a recent article in this series we saw that there were several ways in which a case of covid-19 could be diagnosed by detecting the presence of the virus SARS-CoV-2—at least, so far as mainstream medicine is concerned:
Electron Microscopy The virus is imaged directly using an electron microscope.
Cytopathic Effect The virus is grown in a cell culture and the cytopathic effect which the virus has on the host cells is observed.
Serology The presence of a virus in an infected organism is detected by monitoring the production of antibodies as a reaction to the presence of the virus (ie antigen).
PCR The presence of a virus is detected by replicating a gene unique to the the virus’s genome.
In this article we will examine the third of these: serology.
Antibodies
The theory of antibodies has become one of the central pillars of Western medicine. The Centers for Disease Control and Prevention (CDC) summarize this theory in the following words:
Immunity to a disease is achieved through the presence of antibodies to that disease in a person’s system. Antibodies are proteins produced by the body to neutralize or destroy toxins or disease-carrying organisms. Antibodies are disease-specific. For example, measles antibody will protect a person who is exposed to measles disease but will have no effect if he or she is exposed to mumps. (CDC)
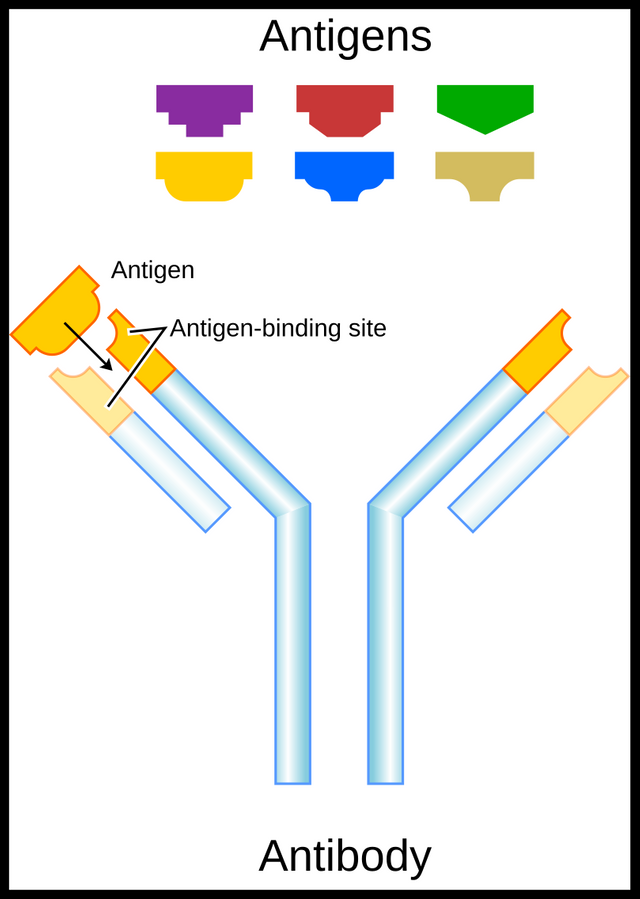
Molecules which stimulate the body to produce antibodies are called antigens:
Present-day vaccines contain a large variety of different molecules which call forth production of complementary antibodies. Because they generate antibody production, we call these molecules antigens. (Nossal 9-11)
What types of molecules can be antigens?
... the most characteristic molecules of living forms are the four great families of macromolecules: proteins, carbohydrates, lipids [fats], and nucleic acids [RNA and DNA]. These are big molecules, composed of many smaller parts; in other words, they are polymers ... Proteins are made up of amino acids, carbohydrates of sugars, and lipids or fats of glycerol and fatty acids. Nucleic acids are more complex and consist of nucleotides strung together; each nucleotide consists of a phosphate group, a sugar, and a base ... If we think, in three-dimensional terms, of a portion of a macromolecule consisting of three to ten average-sized building blocks such as sugars or amino acids, we obtain a picture of one unit of antigen, or in technical terms, one antigenic determinant. It is an area or contour of this size which locks with one molecule of antibody ... Virtually no work of an immunological nature has been done with fats, but each of the other three classes of macromolecules can act as antigens. (Nossal 11-12)
Since 1978, when the second edition of Nossal’s Antibodies and Immunity was published, some lipids have been added to the list of antigens.
The distinction between antigen and antigenic determinant should be noted:
Now as one molecule of protein, for example, can contain hundreds or even thousands of component amino-acid units, clearly a single molecule of antigen can, and usually does, contain a number of antigenic determinants. We are now in a position to define our terms: An antigenic determinant is a molecule or portion of a molecule capable of binding firmly to the combining site of an antibody; an antigen is a molecule containing one or more antigenic determinants. (Nossal 12)
The next term we need to understand is immunogenicity:
Another property of antigens, not possessed by all, is the capacity to call forth antibody production. This property we describe with the clumsy word “immunogenicity.” Let us take a simple example. One protein known to most people is egg white, technically known as ovalbumin. Like most proteins, ovalbumin is an antigen; that is, it can react with specific antibody molecules directed against it. The serum of a normal rabbit will not contain antibodies to ovalbumin. When we inject a solution of ovalbumin under the skin of a rabbit, it will, within a few days, make specific antibody, and if we bleed it the serum will contain numerous molecules of antiovalbumin. Therefore, the ovalbumin is immunogenic in the rabbit. However, if we inject ovalbumin into a normal chicken, we are injecting one of the chicken’s own bodily constituents, and no antibody formation results. In other words, the ovalbumin is not immunogenic in the chicken. (Nossal 13)

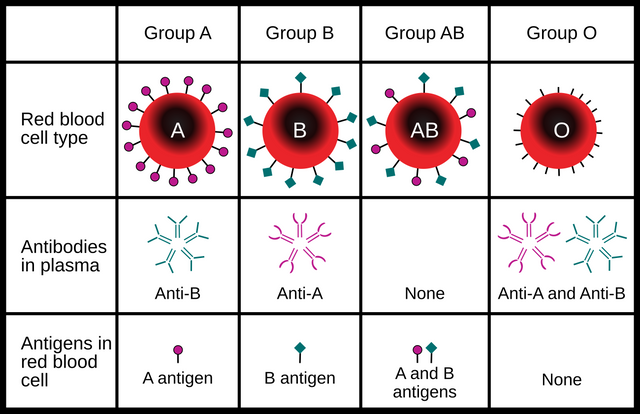
In the case of infectious diseases—which are supposedly caused by pathogenic microbes such as viruses, bacteria or unicellular organisms—the antigens are molecules peculiar to these pathogens. The spike proteins on the surface of SARS-CoV-2 are an example of such antigens:
We have seen that a single antigenic determinant is only a small portion of an antigen molecule. Similarly, a single antigen molecule is only a minute fraction of a pathogenic microbe. A small virus particle, such as poliomyelitis, contains many different kinds of antigens, and thousands of molecules of each kind. A single bacterium, such as typhoid bacillus, contains many more. A preparation containing antigens from microbes or microbial products, useful in the prevention of some infectious diseases, is known as a vaccine. (Nossal 15)
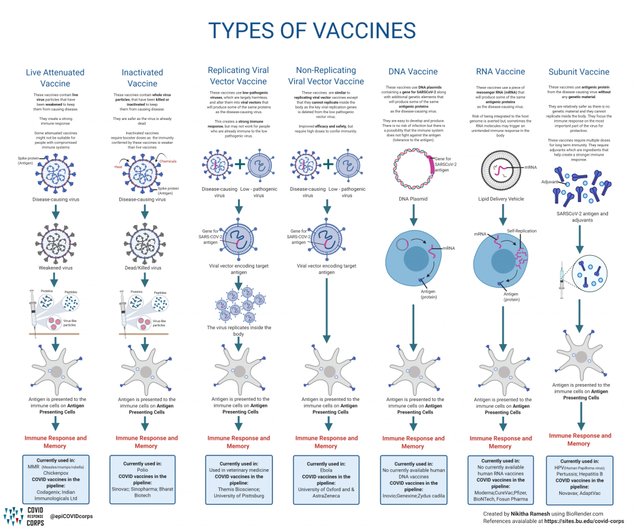
There are three basic types of vaccines:
Dead Viruses
Modified Toxins
Attenuated Microbes

The simplest to understand is the class exemplified by Salk vaccine. This consists of poliomyelitis virus particles that have been killed by formalin. Obviously, a dead virus cannot multiply and infect a living host. However, provided care is taken in the killing process, the antigen molecules of a virus or bacterium are not significantly affected. When injected into a person, they are immunogenic and cause antibody production even though no infection results from their injection.
In the second class of vaccines the antigen consists not of the whole microbe but of modified poisonous material made by the microbe. For example, diphtheria bacilli ... secrete, while they grow, a poison known as diphtheria toxin ... Quite small doses can kill a child. Again, fairly mild chemical treatments can detoxify such poisons. For example, gentle heat and formalin treatment can change diphtheria toxin into a harmless “toxoid,” which has lost its pharmacological power but retains its immunogenicity ...
The third type of vaccine is perhaps the best of all. It is termed a live, attenuated vaccine. Such vaccines consist of living bacteria or viruses which actually infect and multiply in the tissues of the host. However, they are really only cousins of the natural, virulent microbes. By laboratory manipulations, generally involving growth of the microbe in a strange environment, the immunologist has produced genetic variants of the original strain. These are antigenically similar to the disease-causing organism, but lack much or all of their ancestor’s virulence. (Nossal 15-16)
In the years since Nossal wrote this the number of vaccine types has increased, but the underlying principle remains much the same as in his day: antigens stimulate the production of specific antibodies.
In the West, the origins of modern vaccine theory can be traced to the work of Edward Jenner in the 18th century:
An eighteenth-century English milkmaid unwittingly discovered the first antigen. She pointed out to the English general practitioner, Edward Jenner, the odd observation that milkmaids who had caught cowpox (vaccinia) from a member of her herd never subsequently came down with the dreaded smallpox (variola). Jenner was impressed, and intrepidly tested her theory. He inoculated human beings with fluid from a cowpox sore, which resulted in a mild condition only. Indeed, the treatment conferred protection from the infinitely more serious related disorder. Although these studies were well documented and controlled, they were a real shot in the dark. Jenner lived in an age when no one knew about viruses or the true nature of infections. For this reason immunity research lay static for a century, in fact until our golden age. However, so important historically and practically was Jenner’s work that we have come loosely to term all immunization procedures by the word which describes Jenner’s procedure—vaccination ...
We now return to our fabled milkmaid. Inadvertently, she had noted an antigenic relationship between the vaccinia and variola viruses. though by no means identical, these two viruses share certain antigenic determinants. They are sufficiently similar in that antibodies made against one [of the viruses] will prevent the multiplication of the other. Although the crude cowpox fluid used by Jenner was less refined that the present vaccine lymph, the basic principle of this form of immunization remains unchanged. (Nossal 9 ... 16)
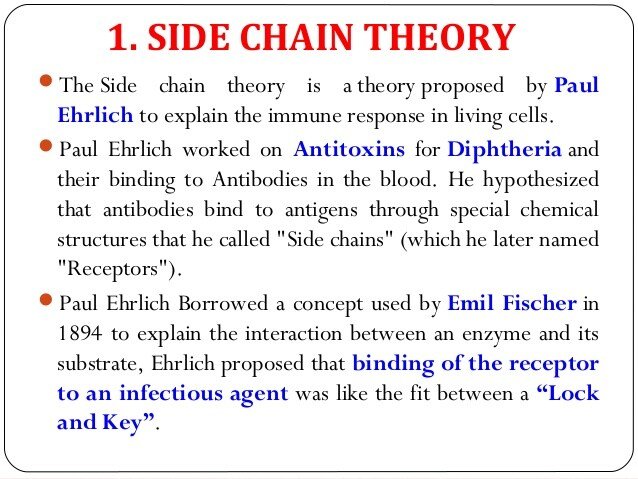
Today, the dominant model of antibodies is the Side-Chain Theory, which was first proposed by Paul Ehrlich in 1897. This is the familiar lock-and-key model, which is currently favoured by many immunologists. Antibodies are constructed with specific receptors, or side-chains, which can bind chemically to antigen determinants on antigens.
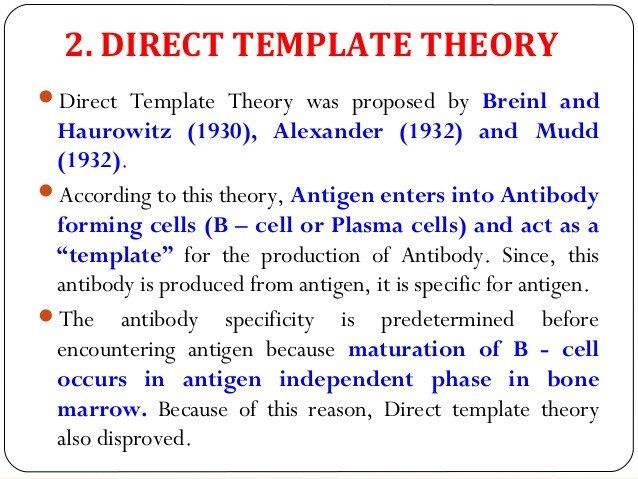
Even among mainstream academics, however, many biochemists have opposed this model. In the 1930s several scientists proposed a variety of mechanisms known collectively as the Direct Template Theory. Antigens enter B lymphocytes—special cells that can create antibodies—and their antigen determinants act as templates for the manufacture of antigen-specific antibodies. This is now considered discredited.
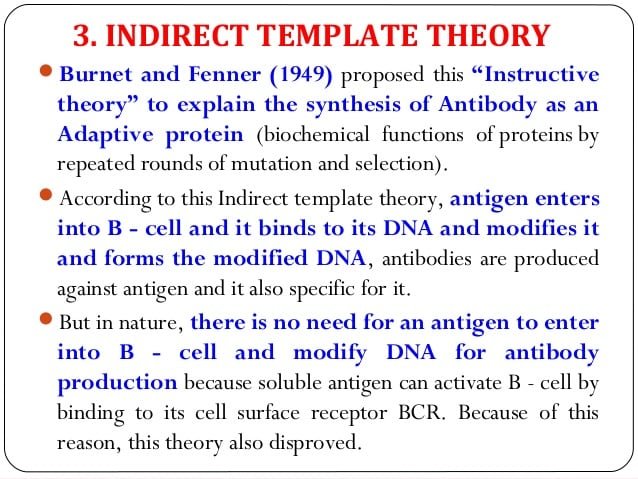
In 1949 Frank Macfarlane Burnet and Frank Fenner proposed the Indirect Template Theory, in which the antigen determinants act as templates not for the production of antibodies but for the alteration of the B cells’ DNA. This model has also been rejected for various reasons.
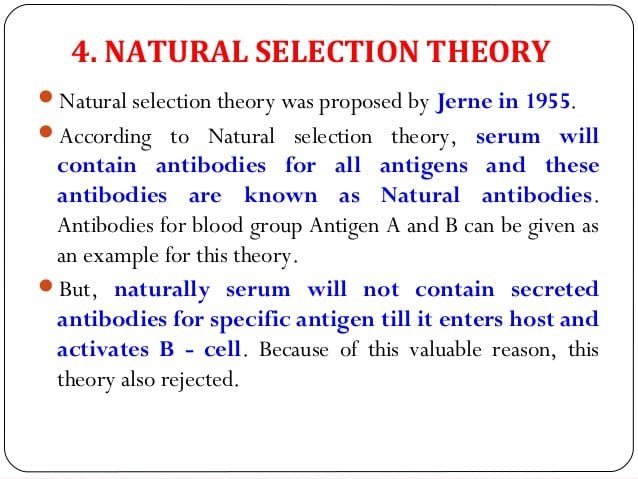
In 1955 the Danish immunologist Niels Kaj Jerne proposed the first of three important theories that would eventually win him a share of the 1984 Nobel Prize in Physiology and Medicine: the Natural Selection Theory. Jerne postulated that the immune system already has all the specific antibodies it needs to fight pathogenic antigens. The argument was that humans who did not have a specific antibody would succumb to the disease associated with that antibody, leaving those who had that antibody to reproduce and pass it on to their progeny. This theory, however, has not stood the test of time. Experience shows that serum does not contain the antibodies for a specific antigen before the individual is exposed to that antigen.
In 1959, Frank Macfarlane Burnet proposed the Clonal Selection Theory. This hypothesizes that a B lymphocyte has receptors specific to a distinct antigen before the body ever encounters that antigen. This hypothesis has become a widely accepted model of the body’s immune response to infection, as it explains how certain types of B and T lymphocytes are selected to destroy specific antigens. Like many of the other theories, it incorporates Ehrlich’s lock-and-key model to ensure that antibodies are antigen-specific.
In 1971, Jerne put forward the second of his three theories:
With his second theory, first set forth in 1971, Jerne sought to explain how the immune system learns to distinguish self from non-self. Immunologists at the time thought that the body’s self-tolerance could not be inherited as a standard pattern but must be learned. Jerne theorized that this “learning” takes place in the thymus gland in the upper chest, where different populations of lymphocytes are exposed to histocompatibility antigens. Lymphocytes that recognize self-antigens are suppressed, whereas non-self lymphocytes, which have accumulated spontaneous mutations, develop and multiply into lymphocytes that can detect foreign antigens. (Page 5)
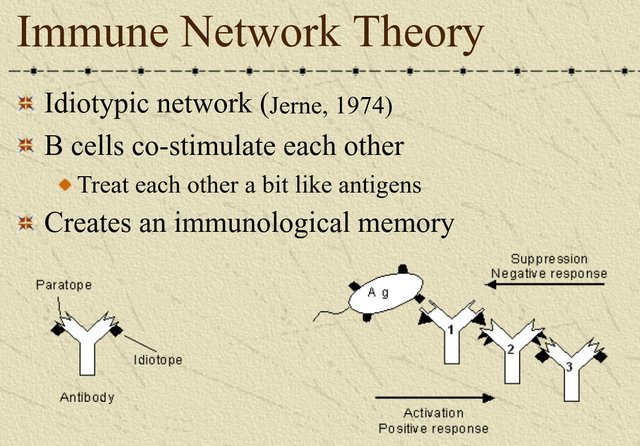
Finally, in 1974 Jerne published his third and most significant theory, Immune Network Theory, which revolutionized the way immunologists thought about adaptive immunity and immune regulation. According to this theory, antibody receptors are attracted to both specific antigens (known as idiotypes) and to other antibodies that bind to the same antibody receptor. The antibodies are in balance until an antigen disturbs the balance, which stimulates the body’s immune response.
Challenging the Orthodoxy
The widely-accepted theory of antibodies has been questioned by some scholars. The foremost among these is perhaps the German microbiologist Stefan Lanka. His paper Die Fehldeutung der Antikörper—The Misinterpretation of Antibodies in the English translation by Northern Tracey & John Blaid—opens with the following claim:
A closer look at antibodies is more important today than ever. After showing in my other articles that there is no proof of the existence of a pathogenic virus, because none of the claimed pathogenic viruses have fulfilled Koch’s postulates, the “antibody” card has now been played by the vaccination advocates. Their claim (which has been drilled into heads for decades) that they are the indirect proof of a pathogen, or offer protection against a pathogen X, is based on an error. This assertion has been repeatedly exposed as false. Since being asked again and again what these antibodies are, I would like to show in this article that antibodies are no proof of protection, nor that they work specifically as in the key/lock theory. (Lanka 1)
Lanka’s explanation of the true purpose of antibodies is a quotation taken from a video that can be viewed on YouTube (in German). Note that in this context titer refers to antibody titer, the concentration of an antibody in the body’s blood serum:
What is a titer increase?
Dr. Stefan Lanka: “The increase is nothing more than the body’s reaction to poisoning [adjuvants]. When the body is poisoned, holes are torn in the cells by these poisons and the cells are destroyed. The body’s reaction when cells break down is to form sealing substances (globulins), small protein bodies that immediately expand in acidic environments, become flat and cross-link with their hydrogen sulphide groups (in which energy is stored) with other proteins and other things.
These cause blood to clot and wounds to heal and they seal our cells when toxins are injected into the body. Even if you get a blow on a muscle, (forming a bruise) or a blow on the kidney (especially sensitive), or the liver, there is an immediate increase in titer. The body reacts to this by sealing the damaged cells and sealing growing cells.
It’s like a house that leaks until the windows are in and sealed. They called this an antibody and even a specific antibody, which is not true. The binding property of these hydrogen sulfide-type proteins is non-specific, they bind to all sorts of things. You can manipulate this in the laboratory by changing the acid level, adding detergents that change the mineral concentration to achieve a binding or not.
The blood of a pregnant woman is full of globulins to seal the placenta, which is constantly growing, to accommodate the baby. The blood of a pregnant woman has to be diluted forty times to avoid a massive positive result in tests, such as an HIV test.” (Lanka 1)
Mike Stone of ViroLIEgy goes even further:
It is very important to understand that when the scientific community and the MSM talk about antibodies, they are speaking about particles never proven to exist. Like “viruses,” antibodies have never been purified/isolated directly from humans nor have they been EM imaged from completely purified samples where these tiny proteins are separated from everything else. They are assumed to be 10 nm in size which is much smaller than most “viruses.” For comparison, “SARS-COV-2” is said to range anywhere from 50 to 200 nm. Indirect methods such as complement fixation, neutralization assays, immunoprecipitation assays, ELISA tests, etc. are chemical reactions used to “detect” the unseen antibodies in order to claim these particles are present yet there are no methods of direct detection. Contrary to the claims, there is zero direct evidence as to whether or not these particles exist. (ViroLIEgy)
Among the problems that beset the orthodox doctrine of antibodies, Lanka and Stone adduce the following:
Some infectious diseases attributed to pathogenic viruses do not require antibodies to protect or immunize an infected person.
There is no correlation between the concentration of antibodies provided by vaccination and the efficacy of the vaccine.
Many people who are vaccinated against a particular disease and as a consequence develop high levels of antibodies subsequently become ill with the very disease they were vaccinated against.
Some diseases (eg measles) may be caught once and never again in one’s lifetime, while other diseases (eg common colds, influenza) may be caught repeatedly over the course of one’s lifetime. Why do the measles antibodies continue to circulate, providing lifelong immunity from a repeat infection, while the influenza antibodies don’t seem to serve any protective purpose whatsoever? If the answer is that the influenza virus keeps mutating, so that repeat infections are really being caused by novel strains of the virus, then we must ask: why does the influenza virus keep mutating but not the measles virus?
If vaccinia (cowpox) stimulates the body to produce antibodies that also prevent the multiplication of the variola virus (smallpox), why then does variola virus not stimulate the production of the same antibodies, protecting the infected person from smallpox? We are told that Jenner’s vaccination worked because vaccinia shares certain antigenic determinants with the variola virus. Why do these antigenic determinants stimulate the production of antibodies when they are part of the vaccinia virus but not when they are part of the variola virus?
Viruses are not alive, so how can a vaccine be made from dead virus? Today, vaccinologists get around this difficulty by saying inactivated virus instead of Nossal’s dead virus.
How many antibodies ensures protection or immunity? If someone is vaccinated but has low levels of antibodies, or none at all, does this mean that the vaccine did not work? What about the case where someone is vaccinated and develops high levels of antibodies, but still gets sick? If someone has too many antibodies, does that mean they have an autoimmune disease due to an overactive immune system? If someone has too few antibodies, do they have a weakened immune system?
The answer to all of these questions: THEY DON’T KNOW. (ViroLIEgy)

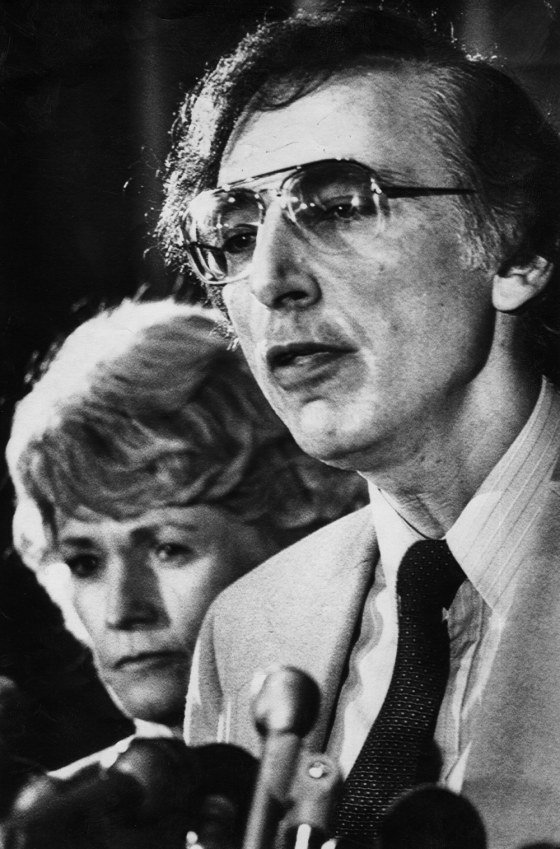
Another antibody skeptic, Tom Cowan, has noticed how the presence of antibodies was once regarded by doctors as proof of immunity from the relevant disease, whereas today patients are tested for antibodies to determine whether they have the relevant disease or not:
Not long ago I had lunch with a homeopathic physician, and we were joking about our respective long careers in medicine, and how much things have changed over the years. For some reason, the conversation turned to immunology, and we asked each other what we remembered learning in medical school about immunology—that was back in the early 1980s. We both jokingly concluded that the only thing we remember was being taught that if you wanted to know whether a patient was immune to a particular viral disease, you could test antibody levels. If the antibodies were high, that meant they were immune.
Just as people remember for the rest of their lives the moment they heard that JFK was shot, or about the World Trade Center towers coming down on September 11, I have a vivid memory of hearing the announcement by Robert Gallo in 1984 that they had found the cause of AIDS. It was caused by a virus called HIV, and the reason they knew it caused AIDS is that they found elevated antibody levels in some (not all) AIDS patients. I remember turning to a fellow medical student at the time and saying, “Hey, who changed the rules?” In other words, after having spent the previous four years learning that people with antibodies to a virus were immune to that particular virus, we were now being told—with no explanation whatsoever—that antibodies meant that the virus was actually causing the disease. (Cowan & Morell 19-20)
What Cowan says of AIDS can equally be applied to COVID-19. If a patient is found to have antibodies against COVID-19, it does not follow that they are immune:
This antibody test can determine whether your body has naturally produced antibodies in response to a past Covid-19 infection, or whether your immune system has developed antibodies following vaccination. This is a quantitative test which means that your results will provide a numerical value for the level of antibodies present. Therefore, by testing again in the future, you can monitor your antibody levels over time ...
Your results will indicate whether you have had Covid-19 in the past and produced antibodies in response, or you have developed antibodies due to the vaccine.
Research suggests that the presence of antibodies may provide protection to Covid-19 for up to six months. However, the link between antibodies and immunity has not yet been confirmed. You may still be able to pass the virus to others or catch the virus again. (Better2Know)
Or again:
Mater Private uses a simple blood test to determine whether antibodies to COVID-19 are present in the blood whether due to natural infection or due to vaccination. For determining antibody response to natural infection, if the initial screening test is positive, a second test is performed to confirm the initial result and to determine the levels of antibodies present. Further clinical advice can be provided by our expert team of clinical microbiologists to determine whether a positive antibody result may be due to a current or a previous infection. For determining antibody response to vaccination, the level of antibody produced in response to vaccination can be measured.
Please note, antibody tests are not recommended for diagnosing active infection with the COVID-19 virus. In addition, there are currently no international guidelines available to indicate what level of antibody produced confers immunity. For this reason, all public health advice should continue to be adhered to regardless of the test result. Symptomatic patients should consult their GP for clinical advice and to arrange testing as needed. (Mater Private Network)

And again:
The antibody test is best done 14-21 days after your first symptom(s). The antibody test is both sensitive and specific to the IgG antibody of COVID-19. A positive test result indicates you have had the virus. However, it is not yet known whether this grants any immunity to the virus. (D2medical)
And finally:
The level of antibodies does not necessarily directly relate to the level of protection any individual may have attained. It is also important to understand that not every individual actually creates circulating antibodies even after confirmed infection or after the vaccine.
Warning: The presence of antibodies does not necessarily mean that the individual is protected against future attacks of Covid-19. (Tropical Medical Bureau)
These quotations are taken from the first four results of the Google search “covid-19 antibody test”, made from a location in Dublin, Ireland.
It is clear that the subject of antibodies and their rôle in immunity is much more involved than the cartoon version we find on Wikipedia and in the mainstream media.
And that’s a good place to stop.
References
- Tom Cowan & Sally Fallon Morell, The Contagion Myth, Skyhorse Publishing, New York (2020)
- Edward Jenner, An Inquiry into the Causes and Effects of the Variolæ Vaccinæ, a Disease Discovered in some of the Western Counties of England, Particularly Gloucestershire, and Known by the Name of the Cow Pox, Sampson Low, London (1798)
- Gustav Joseph Victor Nossal, Antibodies and Immunity, Second Revised and Expanded Edition, Basic Books, Inc, New York (1978)
- Stefan Lanka, The Misinterpretation of Antibodies, Translated from the German Die Fehldeutung der Antikörper by Northern Tracey & John Blaid, Telegram, Online (2020)
Image Credits
- COVID-19 Poster: © 2021 Dublin Region Homeless Executive, Fair Use
- The Lock-and-Key Model of Antibodies: Fvasconcellos (designer), Public Domain
- Blood Group Antigens and Antibodies: InvictaHOG (designer), Public Domain
- Ovalbumin: ChemSrc (designer), Public Domain
- Jonas Salk, Creator of the First Polio Vaccine: Bettmann/Corbis Archive, Fair Use
- Types of Vaccines: © Nikitha Ramesh (designer), Fair Use
- Edward Jenner: Anonymous Portrait, Wellcome Library, Public Domain
- Immune Network Theory: © Jonathan Timmis, An Introduction to Artificial Immune Systems, Fair Use
- Stefan Lanka: © Coronadatencheck, Fair Use
- Mike Stone: © Tom Cowan, Fair Use
- Tom Cowan: © Tom Cowan, Fair Use
- Robert Charles Gallo Announces the Probable Cause of AIDS: Associated Press, © Lana Harris (photographer), Fair Use
- Mater Misericordiae Hospital, Dublin: © The Mater Foundation, Fair Use
Online Resources
