Link to study: https://www.medrxiv.org/content/10.1101/2021.05.11.21256972v1.full.pdf
This is a really interesting study on an aspect of immunity to SARS CoV-2 that to my knowledge has not been examined anywhere else.
While we have seen many studies on virus neutralization (physical blocking of infection) by antibodies, neutralization is only one of three ways that antibodies can protect you from a pathogen. The other two are: 1) phagocytes like macrophages or neutrophils can "feel" the antibodies on the surface of something and thereby know that it something that needs to be eaten 2) Antibodies bound to the surface of something activate complement. Complement then releases molecules that phagocytes can "smell," drawing them to the area. It also adds another flag to the pathogen so that the phagocytes know that it's something that needs to be eaten. In addition, complement can directly kill the pathogen by poking a hole in its cell membrane.
Macrophages are scattered throughout your internal organs and the lining of your mucous membranes. About one in 10 of the cells in your lungs are macrophages. So anywhere a virus lands in there it is going to be close to a macrophage.
These two other means of getting rid of pathogens are relevant to the variants, because the mutations in the variants of concern are clustered in the receptor-binding domain of the spike protein. Changing the part of the protein that binds to the receptor means that neutralization, blocking binding to the receptor, gets harder.
But activation of phagocytosis and complement are not dependent on the antibodies binding to any particular part of the protein. An antibody that has no effect on neutralization might still be able to prevent infection through one of the other two means. And this has not been measured at all.
This study examines all three methods for antibody-based immunity. They are not looking at variants, unfortunately, but they are comparing the antibody function from vaccinated (with the RNA vaccines) people to those with immunity from infection.
The result was that while antibodies from the two groups had similar ability to neutralize the virus, those from vaccinated people were much better at stimulating macrophages to eat spike-coated particles, and activating complement in the presence of spike. The idea is that the antibodies bind (or not) to that spike and have these downstream effects.
The increase in hungry macrophages was explained by the higher overall antibody levels after vaccination. It's not that each antibody was better at stimulating macrophages, just that there were more of them.
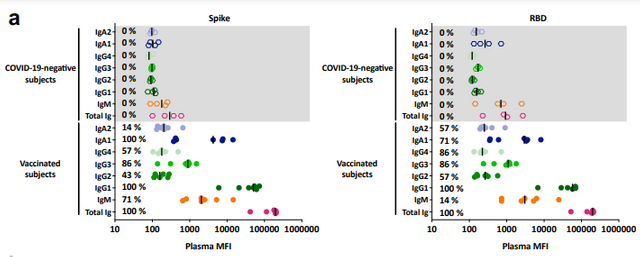
The increase in complement activation, though, actually was not just the increase in antibody numbers. There are different kinds of antibodies; some can activate complement and some can't. The types that activate complement (IgG1 and IgG3) are more prominent in vaccinated people as compared to those with immunity from infection.

The figure above shows the antibody types and functions for the people in the study. Each person is one row. Complement activation on the far right is clearly a lot better for the vaccinated people, as is stimulation of macrophage eating.
The next step would be to do these experiments with variants, to see how well vaccine-induced antibodies stimulate hungry macrophages and activate complement when the spike protein is a variant. Still, this is a very cool study, and I hope to see more like it.