According to the science of virology, viruses are generally too small to be seen with an optical microscope. Although there are some exceptions to the rule, most viruses are said to be 20-200 nm across. This is less than the wavelength of violet light, which means that they cannot be imaged using visible light. They can be imaged, however, in electron microscopes. An electron microscope uses electron waves of smaller wavelength than visible light, which allows it to see objects invisible in optical microscopes.
The electron microscope, therefore, represents the ideal instrument to prove that viruses exist. It may not tell virologists anything about the pathogenicity of viruses, or prove that they are the causes of such ailments as the common cold, influenza, measles, rabies, or COVID-19. At the very least, however, electron microscopy could confirm that the pathogen they claim to have isolated is present in their infected tissue cultures but not in their control cultures.
First Steps
I would go further than this. I would assume that scientific curiosity alone would induce virologists to examine bodily fluids taken from sick people with an electron microscope without first culturing them in the laboratory—without, in fact, doing anything to them other than what is absolutely necessary to prepare a sample for imaging in an electron microscope.
If, for example, rabies is indeed caused by a Lyssavirus, then surely the saliva of a rabid dog must teeming with billions of virions. If a sample of that saliva were imaged in an electron microscope, we ought to see hundreds or thousands, or even millions, of rabies virions. Has this ever been done?
And if measles is caused by a Morbillivirus, as is currently claimed, then surely the pustules that form on the skin of a child suffering from measles must be full of virus-infected pus. Has this pus ever been examined in an electron microscope to see what is in it?
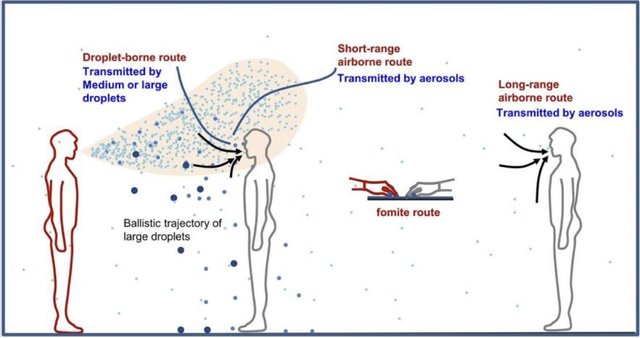
And if COVID-19 is so contagious that we were required to wear masks during the pandemic and to practise social distancing, then surely a single aerosol expectorated out by a COVID-positive patient would be teeming with SARS-CoV-2. Estimates vary, but one online source claims that _The droplets from a single cough or a sneeze emitted by an infected person may contain as many as 200,000,000 virus particles (ClinLab Navigator). Have any electron microscopists examined such sputum?
To my mind, experiments such as these are the obvious first step a virologist should take before moving on to more elaborate experiments, such as tissue cultures and the like. If the resulting electron micrographs show that the infected samples are indeed teeming with virions, while uninfected controls are free from the virus, then a firm link will have been established between the virus and the disease—though the possibility remains that the virus was produced by the disease and not the other way round. If, on the other hand, the micrographs show no virions, then the question must be asked: Why not?
I say first step, but perhaps these experiments should be the second step. A better first step would be to subject these infected bodily fluids to mass spectrometry, or some other method of chemical analysis. Such an analysis might not turn up anything suspicious or pathogenic, but surely any scientist would be curious to learn just what these bodily fluids contain?
Recently, mass spectrometry has actually been adopted by some virologists as a laboratory tool, but it has only been applied to samples of cultured viruses in order to estimate their masses and chemical constituents. It is claimed that viruses may be identified and variants distinguished by identifying their characteristic proteins via mass spectrometry. To my knowledge, however, mass spectrometry has never been used in a clinical setting to simply analyse a sample of infected fluid. Nor has the technique been used to discover a novel virus.
Before one can state definitively that a particular disease is caused by a particular virus, one must first rule out the possibility that the disease is being caused by a non-biological toxin. Mass spectrometry and chemical analysis are the obvious tools to do this. Has this ever been done?
This is a subject we will return in a later article. In the meantime, let us return to electron microscopy.
Misidentification
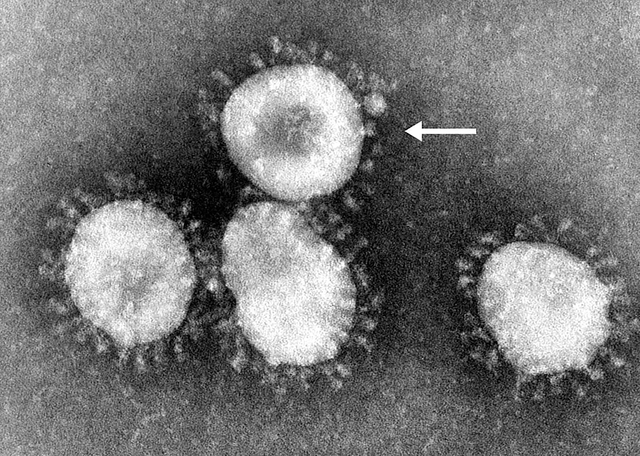
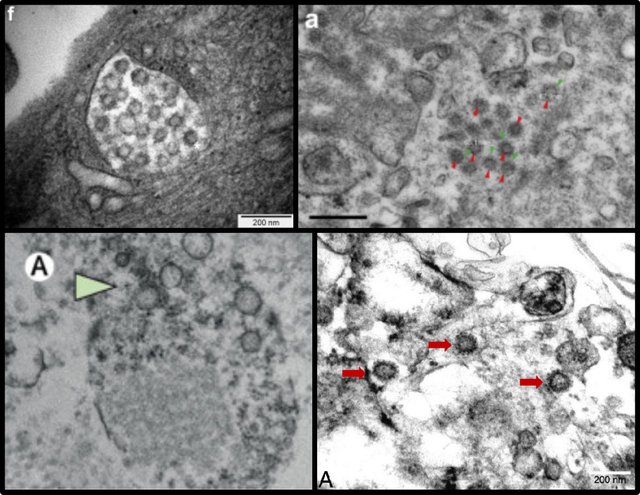
In virology, electron microscopy is generally only used to confirm the presence of a virus that has already been isolated—allegedly—via the standard method of culturing infected tissue samples and observing the cytopathic effect. What do the resulting electron micrographs show? Above is one such micrograph containing subcellular bodies that the researchers have identified as virions of SARS-CoV-2. The scientific literature can provide many similar examples.
But are these really images of SARS-CoV-2? Even in mainstream academia several peer-reviewed papers have been published recently which either warn against hastily identifying such bodies as virions or outright deny that they are virions. For example, in May 2020 The Lancet published a letter to the journal authored by Cynthia S Goldsmith of the Centers for Disease Control and Prevention (CDC) et al which disputes claims made by other researchers that they have demonstrated the infection of epithelial cells by SARS-CoV-2:
... we believe the EM images in the Correspondence do not show coronavirus particles but instead show cross sections of the rough endoplasmic reticulum (RER) ... Just recently, there have been two additional reports in which structures that can normally be found in the cytoplasm of a cell have been misinterpreted as viral particles. EM can be a powerful tool to show evidence of infection by a virus, but care must be taken when interpreting cytoplasmic structures to correctly identify virus particles. (Goldsmith et al e99)
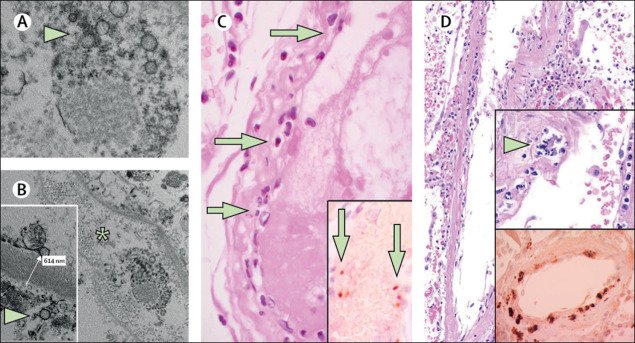
Another example can be found in the Journal of the American Society of Nephrology:
We are concerned about the erroneous identification of coronavirus directly in tissues by authors using electron microscopy. Several recent articles have been published that purport to have identified severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) directly in tissue. Most describe particles that resemble, but do not have the appearance of, coronaviruses. (Miller & Goldsmith 2223)
The offending papers cited are:
Kissling S, Rotman S, Gerber C, Halfon M, Lamoth F, Comte D, et al, Collapsing Glomerulopathy in a COVID-19 Patient, Kidney International, Volume 98, Issue 1, Pages 228–231, Elsevier, Paris (2020)
Su H, Yang M, Wan C, Yi L-X, Tang F, Zhu H-Y, et al, Renal Histopathological Analysis of 26 Postmortem Findings of Patients with COVID-19 in China, Kidney International, Volume 98, Issue 1, Pages 219–227, Elsevier, Paris (2020)
Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al, Endothelial Cell Infection and Endotheliitis in COVID-19, The Lancet, Volume 395, Pages 1417–1418, Elsevier, London (2020)
Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, et al, Myocardial Localization of Coronavirus in COVID-19 Cardiogenic Shock, European Journal of Heart Failure, Volume 22, Issue 5, Pages 911–915, (2020)
Appearances Can Be Deceiving
In August 2020 a peer-reviewed paper was published by Kidney360, one of the journals of the American Society of Nephrology. The lead author, Clarissa A Cassol, is a nephropathologist at Arkana Laboratories, in Little Rock, Arkansas:
- Clarissa A Cassol et al, Appearances Can Be Deceiving—Viral-like Inclusions in COVID-19 Negative Renal Biopsies by Electron Microscopy, Kidney360, Volume 1, Number 8, Pages 824-828, American Society of Nephrology, Washington, DC (2020)
The authors of this paper point out that alleged EM images of SARS-CoV-2 are indistinguishable from images of cellular inclusions that have been observed in kidney tissue since before the emergence of COVID-19:
Since the discovery of the causative agent for the novel severe acute respiratory syndrome (SARS)–like pneumonia syndrome pandemic that started in China in 2019 (1,2), a coronavirus named SARS coronavirus 2 (SARS-CoV-2), electron microscopy images have populated the medical literature (2) and media outlets alike displaying the characteristic 60–140 nm round particles surrounded by a “corona” of 9–12 nm distinctive spikes (2). Although many of these images were obtained after “in vitro” infection of cultured cells with SARS-CoV-2 (2) and are thus likely a true representation of viral particles, we have observed morphologically indistinguishable inclusions within podocytes and tubular epithelial cells both in patients negative for coronavirus disease 2019 (COVID-19) as well as in renal biopsies from the pre–COVID-19 era. (Cassol et al 824)
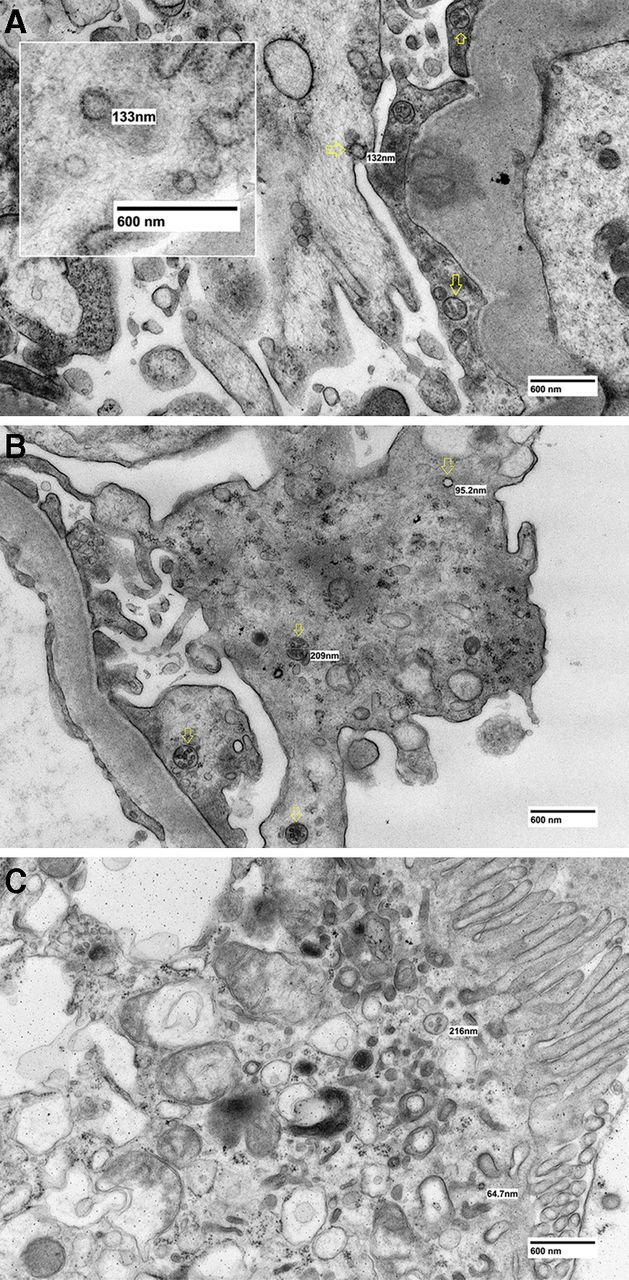
The authors go on to point out that they are not the first to warn of the difficulty in distinguishing between coronavirus particles and naturally occurring subcellular inclusions:
The potential for confusion of coronavirus particles with normal cellular components was in fact highlighted in a detailed ultrastructural study by the Centers for Disease Control and Prevention (CDC) of the SARS-CoV responsible for the 2003 SARS outbreak (9). The authors recommended that, in clinical specimens, the viral nature of inclusions should be confirmed by immunoelectron microscopy for viral antigens or ultrastructural viral RNA in situ hybridization. (Cassol et al 827)
The paper cited—Ultrastructural Characterization of SARS Coronavirus—was published in 2004. But the problem goes back much further than that:
Recognition of this pitfall of “viral-like particles” actually dates back to the 1970s, when the potential for mistakenly assuming that normal cellular components, such as phagocytic vacuoles, microvesicular bodies, or extracellular breakdown products, could represent viral particles was emphasized after a proliferation of studies claiming to have found ultrastructural viral particles within different types of cancer cells and fluids (23). (Cassol et al 827)
The paper referred to is:
- Albert J Dalton, Microvesicles and Vesicles of Multivesicular Bodies Versus “Virus-Like” Particles, Journal of the National Cancer Institute, Volume 54, Issue 5, Pages 1137–1148, Oxford University Press, Oxford (1975)

Tom Cowan, who discusses this subject in his book Breaking the Spell, writes:
Remember the famous “corona” on the coronavirus? It turns out it’s just a common protein that coats normal vesicles and picks up the dyes in the electron microscope preparation. In other words, the “corona” appearance is just another creative fiction dreamed up by virologists and their graphic design team.
The researchers went on to say that, naturally, you see more of these particles in sick people than in healthy people. This is exactly what I have been suggesting this past year [2019-2020]. Dead and dying cells make these particles simply in the dying process and partly to get rid of poisons ...
In summary, the CDC—in 2004—understood that researchers couldn’t reliably know these particles were coronavirus particles. Yet not a word has been heard about this since, and virologists continue to use these pictures as proof of the existence of a new coronavirus. It is a fraud, based on junk science, like everything else connected with “COVID-19.” (Cowan 42-43)
Despite these and similar warnings, misidentification of subcellular bodies has continued, leading Hannah Bullock of Synergy America, Cynthia Goldsmith of the CDC, and three colleagues from the CDC and Duke Medical Center to address the subject in a peer-reviewed paper, which appeared in April 2021 in the CDC’s journal Emerging Infectious Diseases:
- Hannah A, Bullock, Cynthia S Goldsmith, Sherif R Zaki, Roosecelis B Martines, Sara E Miller, Difficulties in Differentiating Coronaviruses from Subcellular Structures in Human Tissues by Electron Microscopy, Emerging Infectious Diseases, Volume 27, Number 4, Pages 1023-1031, Centers for Disease Control and Prevention, Atlanta (2021)
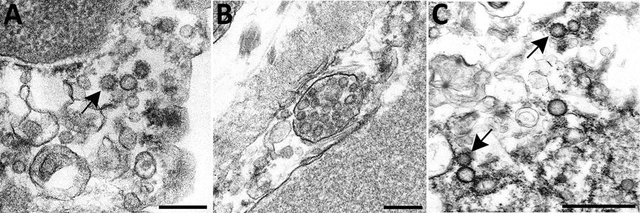
Efforts to combat the coronavirus disease (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have placed a renewed focus on the use of transmission electron microscopy for identifying coronavirus in tissues. In attempts to attribute pathology of COVID-19 patients directly to tissue damage caused by SARS-CoV-2, investigators have inaccurately reported subcellular structures, including coated vesicles, multivesicular bodies, and vesiculating rough endoplasmic reticulum, as coronavirus particles. (Bullock et al 1023)
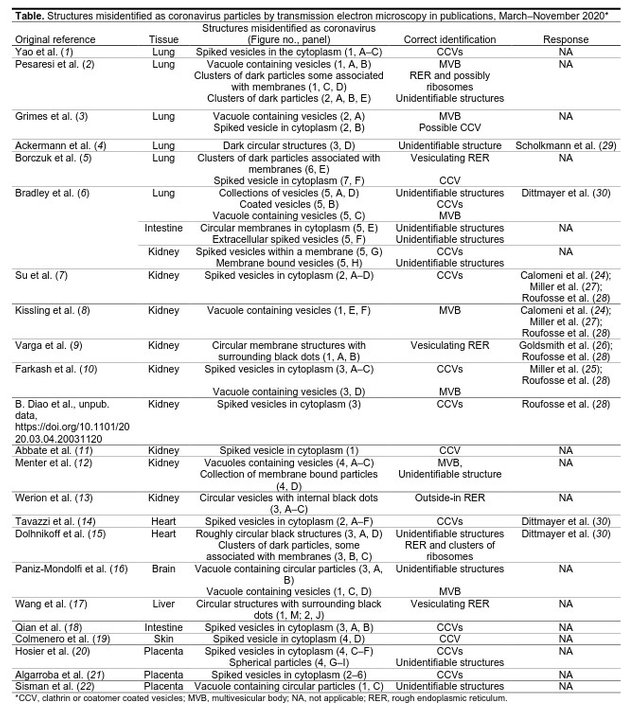
The authors call into question several publications claiming to have imaged the pathogen by electron microscopy (EM):
Consequently, several articles have erroneously described the identification of coronavirus particles by EM in the lung (1–6), kidney (6–13; B. Diao et al., unpub. data), heart (14, 15), brain (16), liver (17), intestine (6, 18), skin (19), and placenta (20–22) (Table). However, most of the presumed virus or virus-like particles shown in all of these reports either represent normal subcellular organelles previously demonstrated in cells (23) or, otherwise, lack sufficient ultrastructure and morphologic features to be conclusively identified as coronavirus. Since early May 2020, letters to the editors of several journals have refuted these descriptions (24–30), yet the misidentification of coronavirus particles continues. (Bullock et al 1023)
The Table on page 1024 lists no less than twenty-two papers that passed peer-review despite containing incorrectly identified electron micrographs. Bullock and her co-authors identified the alleged coronavirus particles as:
MVBs (multivesicular bodies)
Unidentifiable Structures
The authors do not dispute the existence of the SARS-CoV-2 virus or the hypothesis that it is the causative agent of the disease COVID-19. Curiously, though, they never ask the pertinent question:
- If these subcellular bodies in the electron micrographs are not coronaviruses, then where are the viruses? In each of these papers, the samples that were subjected to electron microscopy came from patients who had tested positive for COVID-19 or whose death had been attributed to COVID-19. But if Bullock and her colleagues are correct, the subsequent electron micrographs show that no virus is present, contradicting these claims.
Clones
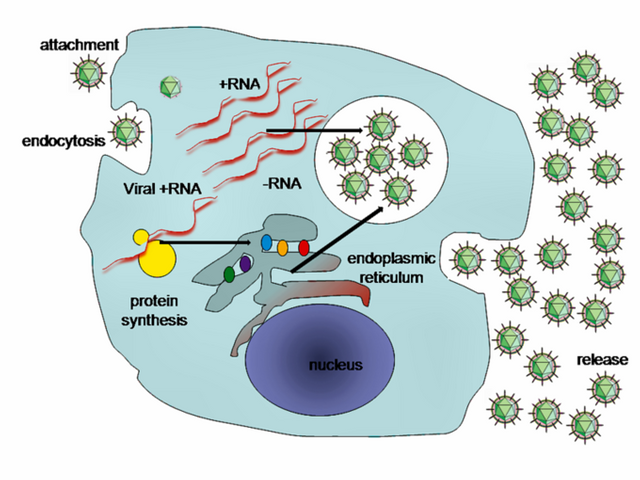
According to virologists, viruses are not living organisms that reproduce by any of the common methods found in the animal and plant kingdoms. Instead, a single virion invades a host cell, somehow takes over the machinery of that cell, and induces it to make copies of the virion using the virion’s genetic material (DNA or RNA) as a blueprint. The resulting virions then burst out of the host cell and go on to invade and infect other cells.
If this scenario is accurate, then each of those daughter virions is a clone of the parent virion that first infected the host cell. Because viruses do not grow or feed like living organisms, these clones ought to be exact copies of the infecting virion: replicants identical in all respects to the latter.
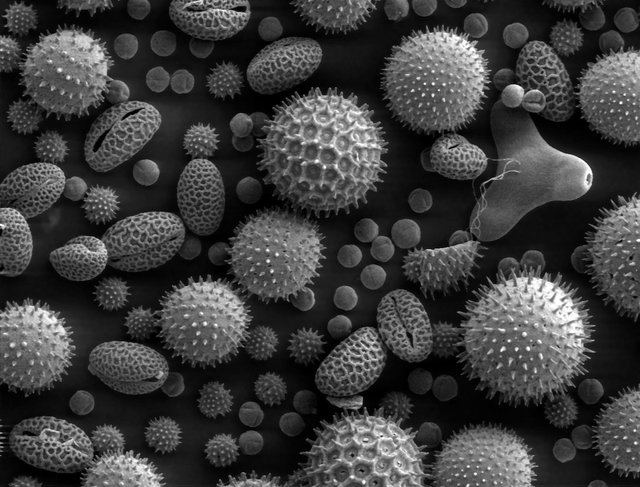
Why, then, do the virions in electron micrographs always display a wide range of morphological characteristics? Their shapes vary from perfectly spherical to irregular in outline. The number and the appearance of the protein spikes also vary greatly. And the size of the virions varies. We are told that each SARS-CoV-2 virion is 60–140 nanometres in diameter (Zhu et al). How could a clone be more than twice as big as its parent?
Admittedly, some of these discrepancies can possibly be explained by the exigencies of electron microscopy:
For diagnostic EM, coronaviruses can be observed using 2 techniques, negative stain and thin section. Negatively stained samples are prepared by adsorbing virus suspended in fluid onto a plastic-coated grid, wicking off excess liquid, and staining with a heavy-metal salt solution. The virus is coated with the stain, which penetrates between spikes protruding on the virus surface, making them visible. Thus, negative stain EM images readily show the prominent spikes that are associated with coronaviruses. For thin section EM, tissues or infected cell culture specimens are fixed in formalin or glutaraldehyde, stained with osmium, embedded in epoxy resin, baked to harden, and sectioned using an ultramicrotome. The resulting ultrathin sections show a cross-sectional view of the cells and viruses. In ultrathin sections of fixed tissues, coronavirus particles are ≈100 nm in diameter including their peplomer spikes and ≈80 nm in diameter excluding spikes. The spikes on coronavirus particles within cytoplasmic vacuoles are not easily visible by thin section EM, unless the tissue is processed with tannic acid; instead, they usually appear as a fuzz on the surface of the virus. The difference in the appearance of the virus in negative stain versus thin section contributes to the confusion and misidentification of coronaviruses. Spikes are very rarely as clear in thin-sectioned specimens as they are when seen by negative stain EM. (Bullock et al 1023-1024, parentheses removed)
But this does not explain the 80-nm discrepancy in size observed by Zhe et al.
Compare the electron micrograph of SARS-CoV-2 near the top of this article with the following EM image of pollen grains. Note how similar the different types of pollen are to one another. One could easily mistake this for a computer-generated image. But these pollen grains are not clones or replicants:
Given the doubts that even mainstream virologists have raised with regard to alleged electron micrographs of viruses, and given the objections raised in this article, I would be very reluctant to base any claim that viruses are real on the evidence of electron microscopy.
And that’s a good place to stop.
References
- Hannah A, Bullock, Cynthia S Goldsmith, Sherif R Zaki, Roosecelis B Martines, Sara E Miller, Difficulties in Differentiating Coronaviruses from Subcellular Structures in Human Tissues by Electron Microscopy, Emerging Infectious Diseases, Volume 27, Number 4, Pages 1023-1031, Centers for Disease Control and Prevention, Atlanta (2021)
- Clarissa A Cassol et al, Appearances Can Be Deceiving—Viral-like Inclusions in COVID-19 Negative Renal Biopsies by Electron Microscopy, Kidney360, Volume 1, Number 8, Pages 824-828, American Society of Nephrology, Washington, DC (2020)
- Tom S Cowan, Breaking the Spell, DrTomCowan.com, Online (2020)
- Cynthia S Goldsmith et al, Electron Microscopy of SARS-CoV-2: A Challenging Task, The Lancet, Volume 395, Issue 10238, Page e99, Elsevier, London (2020)
- Sarah E Miller, Cynthia S Goldsmith, Caution in Identifying Coronaviruses by Electron Microscopy, Journal of the American Society of Nephrology, Volume 31, Issue 9, Pages 2223-2224, American Society of Nephrology, Washington, DC (2020)
- Zsuzsanna Varga et al, Endothelial Cell Infection and Endotheliitis in COVID-19, The Lancet, Volume 395, Issue 10234, Pages 1417-1418, Elsevier, London (2020)
Image Credits
- COVID-19 Poster: © 2021 Dublin Region Homeless Executive, Fair Use
- Alleged Aerosol Transmission of COVID-19: © P V Nielsen & L Liu, The Influence of Air Distribution on Droplet Infection and Airborne Cross Infection, Department of Civil Engineering, Aalborg University, DCE Technical Memorandum No. 77, Aalborg (2020), Fair Use
- Supposed Electron Micrograph of SARS-CoV-2: © Fred Murphy (electron microscopist), Centers for Disease Control and Prevention, Public Health Image Library, Fair Use
- Alleged Electron Micrographs of SARS-CoV-2: © Zsuzsanna Varga et al, Fair Use
- Four Alleged Electron Micrographs of SARS-CoV-2 - A: © Kissling et al (erectron microscopists), Fair Use
- Four Alleged Electron Micrographs of SARS-CoV-2 - B: © Hua Su et al (electron microscopists), Fair Use
- Four Alleged Electron Micrographs of SARS-CoV-2 - C: © Zsuzsanna Varga et al (electron microscopists), Fair Use
- Four Alleged Electron Micrographs of SARS-CoV-2 - D: © Guido Tavazzi et al (electron microscopists), Fair Use
- Viral-Like Particles in Non-COVID-19 Patients’ Biopsies: © Clarissa A Cassol et al (electron microscopists), Fair Use
- Tom Cowan: © Dr Tom Cowan, Fair Use
- Commonly Misidentified Viral-Like Particles: © Hannah A Bullock et al (electron microscopists), Fair Use
- Table of Misidentified Viruses: © Hannah A Bullock et al, Fair Use
- Cartoon Version of Viral Replication: © Course Hero, Inc, Fair Use
- An Electron Micrograph of Pollen Grains: Dartmouth College Electron Microscope Facility, Public Domain
Online Resources
