https://www.nature.com/articles/nature10831
Warnings from epidemiologists and virologists regarding the potential danger of an Avian Influenza virus mutating to become transmissible in humans have finally begun to get traction in the mainstream media. Just so we're clear on why this is important: in humans, the IFR (Infection Fatality Rate) of HPAI (Highly Pathogenic Avian Influenza) is above 50%.
Now that I have your attention --
The question arises: could such a mutation happen? Is there some derivative sequence of Avian Influenza that could arise from the influenza genomes that we currently understand?
First, a little bit of background on Influenza. The capsid (that's the outer protective coating of a virus) of Influenza virions is composed of two proteins, hemagglutinin (abbreviated as H or HA) and neuraminidase (abbreviated as N or NA). There are 18 subtypes of H (numbered 1 through 18) and 137 subtypes of N, 9 of which occur in Influenza virions, with these subtypes being numbered 1 through 9. When you see the name of an Influenza virus, it's almost always something like H1N1, or H5N1, or H7N9, etc. The naming convention reflects the makeup of the capsid, and the H protein of the capsid determines which receptors that Influenza virion can bind to as well as its efficiency at cellular membrane fusion.
HPAI viruses (again HPAI stands for Highly Pathogenic Avian Influenza) typically contain HA subtype 5 (or just "H5") in their capsid. That's good news for us humans because the receptors that H5 binds to aren't present in the nose, mouth, or upper respiratory tract of mammals. That makes it difficult (but not impossible) for a mammal to become infected, and makes it virtually impossible for mammal-to-mammal transmission to occur. Note that mammalian infection is possible, because our lower respiratory tract expresses the appropriate receptors for H5, but mammal-to-mammal transmission is unlikely... which is what protects us mammals from an H5N1 pandemic.
So... could H5 mutate to bind to receptors that are expressed in the upper-respiratory tract of mammals? If it could, the potential death toll from the resulting pandemic could be enormous. (Don't go all doom-and-gloom when you read that sentence... there are significant mitigating factors that we'll discuss)
In 2012, virologist Masaki Imai and colleagues at the University of Tokyo and the University of Wisconsin set out to determine if such an H5 mutation could occur in nature. I want to emphasize to readers at this point that the appropriate biosafety protocols were followed in the experiment I'm about to describe, including intentionally using a genome from a virus that is considerably less lethal in humans than the H5N1 HPAI.
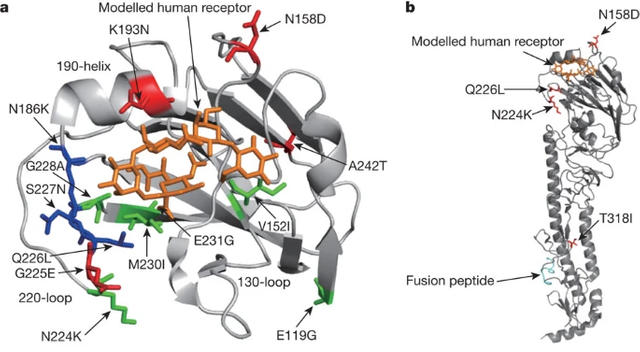
Much like human DNA is divided into 46 groups of segments called chromosomes, Influenza RNA is divided into 8 gene segments. Imai and his team started with the 8 gene-segments of the H1N1 virus (which is infectious and transmissible in humans), and replaced the gene-segment that encodes the HA protein with the homologous (i.e., "matching") gene segment from H5. The resultant "reassortant" genome was mostly H1N1, but with the capability of binding to receptors in the lower respiratory tracts of mammals. It's important to note that this kind of "reassortment" of Influenza gene segments happens regularly in nature, and is a common product of an organism being infected with two different types of Influenza at once. (Pigs, notably, are susceptible to both H1N1 and H5N1)
Using this "reassortant" hybrid virus, Dr. Imai and his team induced a number of random mutations in the HA gene, then built a gene-library of the resulting mutated RNA. I'll skip over some steps here, but after some work, they were able to introduce these mutated H5-bearing viral RNAs into ferrets (which serve as a good respiratory model for humans), place those ferrets in cages next to "control" ferrets, then after a few days test the "control" ferrets to determine whether the H5-bearing influenza had been transmitted to them.
The answer is "yes". Four random mutations were all it took to yield a form of H5 that could bind to the upper respiratory tract in ferrets and become transmissible.
Before continuing on with the virology, I would like to pause for one moment to pose a policy proposal: a significant part of our national defense budget should be being spent on pandemic prediction and prevention efforts. SARS-CoV-2 killed roughly twice as many Americans as the two World Wars combined, and SARS-CoV-2 had an IFR of no greater than 1%.
Back to the virology -- I promised mitigating factors. In the experiments performed by Dr. Imai and team, the resulting virus was infectious and transmissible, but not particularly dangerous. No ferret died from the resulting infection. Another mitigating factor is that we have the capability of producing vaccines against various Influenza viruses. (Though note: the methods of producing vaccines against Influenza all [with one exception] rely on eggs, which could become a liability in an Avian flu epidemic). We are also likely on the verge of being able to mass produce Influenza mRNA vaccines, which would allow us to quickly tailor a vaccine to the specific virus attacking us, and does not rely on eggs.
There are all kinds of reasons the experiments described in the attached paper aren't a perfect analog to a mutated HPAI. That being said, Dr. Imai and his team have given us credible evidence of straight-forward mutations in the H5 protein that have the demonstrated capability of enabling mammal-to-mammal transmission of HPAI... and those mammals are likely to include humans.