I recently wrote a letter to the editor of the journal Burns[1] explaining three reasons why in vitro studies of biofilms will produce conclusions that are not translatable to the real world setting. When scientists test interactive dressings in petri dishes, their conclusions are meaningless, because they leave out too many variables that will influence the results in living humans. The authors of the article to which my letter referred graciously agreed that this is a real problem.[2] A similar problem can be seen in the artificial pressure redistribution demonstration used to sell dressings for closed (Stage I and Deep Tissue) Pressure Injuries.
During the five years I volunteered in a remote area of West Africa, I worked with a patient population who, for the most part, slept on bare ground. I can assure you that such populations are not purchasing dressings for pressure redistribution. The patient these pressure-redistributing dressings are designed for is already lying on an 8” or thicker high density foam mattress; a modern invention which redistributes pressure so well that Bergstrom et al. found that moderate and high risk patients (Braden score 10 – 14) can safely lie in one position for four hours before being turned.[3] Despite this fact, sales representatives told me, with a straight face, that adding the few millimeters of their foam dressing between the patient and the mattress, rather than a dressing that is a little bit softer, is going to make a cost-effective difference in pressure redistribution for these patients. Seriously?
A friend repairs electronics that have been hit by lightning. He laughs when customers lament that their surge protector failed. He explains that surge protectors are for minor electrical spikes from the power company. Lightening is electricity that travels miles across the open sky, from the clouds to your house, and you think a tiny fuse should be able to stop it? It is all a matter of scale. Relatively thin dressings are not, nor will they ever be, an effective support surface.
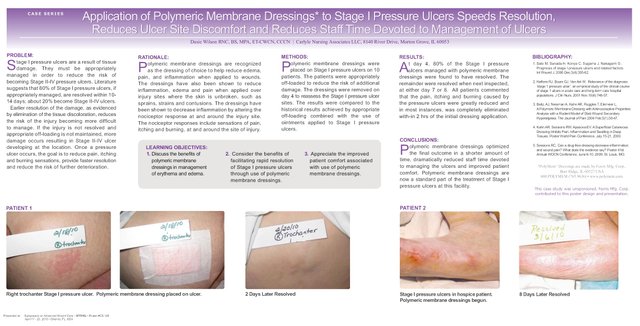
If you want a dressing that will influence outcomes with closed pressure ulcers, do not look for a dressing to alter the pressure redistribution. Rather, choose the dressing type known to address the other underlying cause of pressure ulcers: inflammation. Polymeric membrane dressings (PMDs) are able to decrease the secondary inflammation caused by the nociceptors (pain sensing nerves).[4] Diminishing the inflammation with PMDs can stop the problem in its tracks, and even reverse it. Without excess inflammation, the body stops sending the enzymes that break down the tissue. The capillary leakage that causes the edema is halted as well. Resolution of the edema improves circulation and lymphatic drainage so that the body can remove the irritants and heal the damage.[5] PMDs have been shown, in a clinical cohort study, to consistently resolve Stage I Pressure Injuries without the development of an open wound.[6]
(Linda Benskin, PhD, RN, CWCN, CWS, DAPWCA, is an Independent Nurse Researcher for Rural Areas of Tropical Developing Countries and Clinical Research & Education Liaison, and Charity Liaison for Ferris Mfg. Corp.)
P.S. After I wrote this, I realized that in addition to all the above flaws, the artificial test for pressure redistribution actually shows that the unnamed dressing those sales reps are trying to sell redistributes the pressure exerted on the mattress by concentrating it on the patient's pressure point, rather than the reverse. (For those of you who have seen the demonstration, the steel ball, not the pressure pad, is the part that represents the patient, and the dressing is protecting the pressure pad, which represents the mattress). So, if this stiff dressing makes a difference at all, it will be to increase, not decrease, the risk of pressure injuries. Softness and flexibility are yet more reasons to choose PMDs.
- Benskin LLL. Limitations of in vitro antimicrobial dressings study. Burns. 2016;42(6):1. doi:10.1016/j.burns.2016.01.034.
- Webber MA. Response to Letter to Editor: “Limitations of In Vitro Antimicrobial Dressings Study.” Burns. 2016;0(0). doi:10.1016/j.burns.2016.02.015. in press
- Bergstrom N, Horn SD, Rapp MP, Stern A, Barrett R, Watkiss M. Turning for Ulcer ReductioN: A Multisite Randomized Clinical Trial in Nursing Homes. Journal of the American Geriatrics Society. 2013;61(10):1705–1713. doi:10.1111/jgs.12440.
- Benskin LLL. PolyMem Wic Silver Rope: A Multifunctional Dressing for Decreasing Pain, Swelling, and Inflammation. Advances in Wound Care. 2012;1(1):44-47. doi:10.1089/wound.2011.0285.
- Benskin LL. Polymeric Membrane Dressings for topical wound management of patients with infected wounds in a challenging environment: A protocol with 3 case examples. Ostomy Wound Management. 2016;62(6):42-62.
- Wilson D. Application of Polymeric Membrane Dressings to Stage I Pressure Ulcers Speeds Resolution, Reduces Ulcer Site Discomfort and Reduces Staff Time Devoted to Management of Ulcers. April 2010.