Part 3: Recovering From A Nightmare
This article is the third in a series on psychiatric drugs, the influence of the pharmaceutical industry on both the general public and medical professionals, and the dangers of over-prescription.
Here's a link to my first two articles, in case you missed them:
Part 1: Downward Spiral
Part 2: Planetary Vibe Adjustments
Serotonin Syndrome
In March of 1984, 18 year old Libby Zion arrived at a New York hospital with an unknown flu-like ailment. She had been taking Nardil, a prescribed anti-depressant. In an attempt to control the strange jerking motions she was exhibiting, emergency room physicians administered Demerol, a narcotic painkiller.
The combination of the anti-depressant and the painkiller resulted in her level of circulating serotonin to climb dangerously high. She died soon after of cardiac arrest.
Serotonin Syndrome, sometimes referred to as Serotonin Toxicity, is a life-threatening drug-induced condition caused by excess serotonin within the central nervous system. It results in a wide range of symptoms such as high body temperature, changes in mental status, increased reflexes, tremors, and dilated pupils. Serotonin Syndrome can be fatal, and is considered a medical emergency. If it reaches a point of rapidly increasing temperature and muscle rigidity, multi-organ failure can occur.
Severe cases of Serotonin Syndrome are almost always caused by a drug interaction involving two or more ‘serotonergic’ agents (drugs that regulate serotonin levels), at least one of which is typically an antidepressant such as a selective serotonin reuptake inhibitor (SSRI).
Due to the extremely variable presentation of this condition and the lack of a single diagnostic test to confirm it, Serotonin Syndrome is highly under diagnosed. Many physicians are unaware of Serotonin Syndrome, and symptoms may be dismissed as being unrelated to pharmaceutical treatments.
Finally, An Explanation
By March of 2018, over a year after I started taking the Escitalopram, I still had not recovered. I was only operating at about 25% of normal capacity, and I continued to struggle with unmanageable levels of anxiety.
My cousin mentioned that she'd seen a naturopathic doctor (ND), and that it was helpful in finding the root cause of issues when it's unclear why symptoms are present.
To legally practice in most parts of North America, NDs must complete a four-year, full-time program at an accredited school of naturopathic medicine. (Note that naturopathy and homeopathy are not the same thing).
In general, medical doctors are trained to treat symptoms. There are cases where a medical doctor is clearly appropriate, such as an emergency, a situation where you'd like to relieve symptoms with pharmaceuticals, or if you require a surgical procedure.
The core tenet of naturopathy is to identify and treat the root causes of symptoms. NDs employ a variety of natural treatment methods such as dietary and lifestyle changes, vitamins, supplements and herbal remedies. Many NDs will work with MDs when treating patients. Some cases where a naturopathic doctor would be appropriate would be for mental health issues such as anxiety or insomnia, pain relief, or suspected allergies.
Adrenal Fatigue
I made an appointment, and went in with no expectations. During the appointment I explained everything that happened over the last few years - the stress, the Adderall, and the reaction to the Escitalopram. The ND asked many questions about my diet, lifestyle, and sleeping habits to get a complete picture of my overall well being.
She concluded that chronic, extreme stress resulted in a condition called Adrenal Fatigue. The adrenal glands produce cortisol, a hormone that helps you respond to stress. When stress is extreme or chronic, the adrenal glands can become taxed. This exhaustion of the adrenal glands presents as a set of signs and symptoms including fatigue, difficulty getting up in the morning and increased energy in the evenings, overuse of caffeine or other stimulants, inability to handle stress, weakened immunity, and sleep problems.
There are four stages of Adrenal Fatigue, each with a different combination of symptoms and varying levels of stress hormones. The state of "shut down" I experienced in January of 2017 was the fourth stage of Adrenal Fatigue (the 'Burnout' phase). By the time stage four is reached, levels of cortisol begin to drop. This is the point of finally crashing after a long period of coping with stress, and has implications for almost every part of the body. Recovery from stage four of Adrenal Fatigue requires significant time (sometimes years), and often a complete lifestyle change.
The mainstream medical model recognizes two diseases of the adrenals: Addison's disease (severe adrenal insufficiency) and Cushing's syndrome (extreme overproduction of cortisol). Hormone levels vary from person to person, and they naturally fluctuate throughout the day. This makes it difficult to obtain a conclusive laboratory test for the condition before it reaches a disease state. Conventional medicine acknowledges that the symptoms of Adrenal Fatigue are real, but does not recognize a dysfunction of the adrenal system as long as a test for Addison's disease is negative.
Since many doctors are unaware of Adrenal Fatigue, they often turn their attention to other possible causes that have similar clinical presentations, such as depression. As in my case, this can lead to a misdiagnosis and treatment with medication. This form of treatment may leave the root cause unresolved, resulting in a worsening of the condition over time.
Dangerous Serotonin Levels
When I described my experience during the spring and summer of 2017, the ND immediately recognized it as Serotonin Syndrome.
I was taking Adderall to treat ADHD symptoms when my family doctor prescribed an SSRI. When there were no improvements, she doubled the dose.
Amphetamine, the active ingredient in Adderall, increases serotonin levels. Escitalopram blocks serotonin reuptake. The concurrent use of two serotonergic agents caused dangerous levels of serotonin, and resulted in the extreme symptoms I experienced.
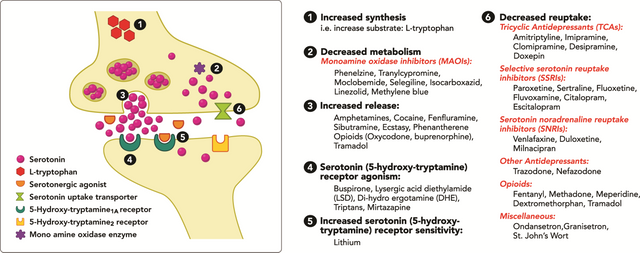
Increasing intrasynaptic serotonin levels: Mechanisms and associated serotonergic agents.
Image Source
Treatment & Recovery
The ND recommended that I reduce stress and rest whenever possible. She highlighted the importance of adequate sleep, and spending time outdoors. She also suggested mindfulness meditation, which has been shown to reduce anxiety and improve concentration.
She recommended a diet of nutrient-dense foods with lots of fresh vegetables and protein, as well as the following supplements:
Multistrain Probiotics: The gut harbours a complex community of microbial cells called the microbiota. The gut microbiota has a profound influence on human health, including digestion, immune function and mental state. Factors such as stress and antibiotic use can disrupt the microorganism population. The use of multistrain probiotics helps to promote the growth of beneficial bacteria, and has been linked to improved symptoms of anxiety and depression.
Omega 3 + Vitamin D (liquid): Omega-3 fatty acids can help alleviate symptoms of depression, anxiety and ADHD. They have been shown to increase the length and quality of sleep, and offer many other health benefits including skin and eye health, reduced inflammation, and improved risk factors for heart disease. Vitamin D is known to influence basic cognitive function, mood, and overall mental health. Studies indicate that there is an association between low Vitamin D levels and both ADHD and depression.
Vitamin B: Vitamin B5 helps support adrenal function, stress response, and healthy immune function. Vitamin B12 and other B vitamins play a role in healthy brain functions, and are important in regulating mood. Supplementation with B vitamins can help alleviate depression and ADHD symptoms.
Albizia: Albizia julibrissin, also known as the Silk Tree or Mimosa, has been used for centuries in traditional medicine. It is helpful in treating symptoms of depression and anxiety.
DT-Matrix: A formulation of herbs, including milk thistle and picrorhiza kurroa (helpful for liver function), as well as bearberry, stinging nettle, and burdock to facilitate kidney function.
Gamma-Aminobutyric acid (GABA) + L-Theanine: The neurotransmitter Gamma-Aminobutyric acid (GABA) helps send messages between the brain and the nervous system. It is linked to anxiety, ADHD and insomnia. L-Theanine is an amino acid known to reduce anxiety, enhance cognitive abilities, and promote relaxation. It can also help regulate cortisol production.
Within days of starting the supplements, I noticed a dramatic improvement. My anxiety level dropped, and my energy increased substantially. Over the next two months, my energy and mental state improved further. My skin became clearer and more even toned. I continue to notice improvements daily.
This horrific experience has left me with a number of sobering questions. How could this have happened? What gaping hole in this system must exist to allow such a dangerous and life-altering mistake to be made? Considering that Serotonin Syndrome is well documented in medical literature, how is it that both the prescribing doctor and a psychiatrist - a specialist in mental health and psychiatric medication - could be unaware of Serotonin Syndrome as a result of combining a stimulant and an SSRI?
I've spent the last few months researching these topics. In my next article, I will review what I've learned about propaganda techniques used by the pharmaceutical industry, and how it is contributing to the epidemic of over-prescription in North America.







Congratulations @pilgor! You have completed some achievement on Steemit and have been rewarded with new badge(s) :
Click on any badge to view your own Board of Honor on SteemitBoard.
For more information about SteemitBoard, click here
If you no longer want to receive notifications, reply to this comment with the word
STOPDownvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit