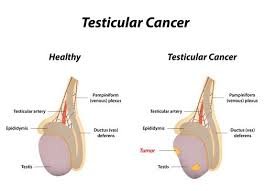
An Overview of Testicular Cancer:

The effective treatment of testicular cancer is dependent on a variety of factors such as early detection, properly diagnose, and treatment type or/and healthcare system. The male testicles are made up different cells and since cancer is associated with or as an abnormal growth of cells. All cells present in the human body can become cancerous. According to the American Cancer Society, (n.d.), Special cells known for their association with the production of sperm are also known to be responsible for an average of ninety percent testicular cancer cases in men. Testicular cancer often contains a mixture of both seminomas and non-seminomas germ cells. However, in the case of testicular cancer, the mixture is considered as non-seminomas due to their growth and spread characteristics (non-seminomas germ cells). On the other hand seminoma, germ cells are responsible for over ninety-five percent of testicular cancers that occur in men from ages 25 to 45. Furthermore up to 8720 cases of testicular cancer is yet to be diagnosed according to the estimates of the American Cancer Society, and about 380 of them will die of testicular cancer.
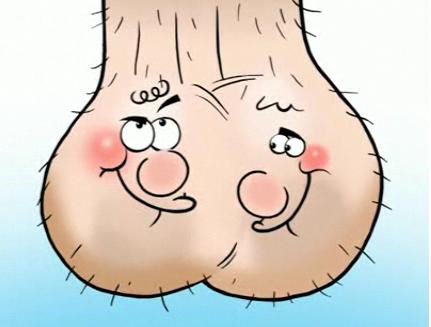
Self-Examination for Testicular Cancer
Self-management of testicular cancer begins with self-examination. The American Cancer society (n.d.) recommends that the best time for self-examination is immediately after a shower when the scrotum is relaxed. The following are steps were suggested for the exercise:
- examining each testicle at a time;
- hold out each testicle out in between one's thumb, fore, and index fingers, then roll gently for a while;
- Check for hard lumps by feeling the surface area of the testicles one after the other, as well as looking at the testicles cautiously to find and inconsistencies in their shape and size.
The second stage of self-management is the treatment stage. Once a man is diagnosed with non-seminoma or seminoma testicular cancer, whether advanced or not it is best to see a physician and begin treatment immediately. There are different treatment approaches recommended by physicians for the management of testicular cancer. It is best to allow a doctor recommend the most appropriate treatment in accordance with the stage of testicular cancer.
Self-management of Seminoma Testicular Cancer
Patients recommended referred for the treatment of seminomas associated cancer must be AFP negative, due to the fact that any elevations of AFP noticed indicates that the cancer cells are not seminomas but are rather non-seminomas (Cancer Care Nova Scotia, 2005). However, mild ßhCG and LDH elevations are acceptable. If a patient's pathological review exhibits pure seminoma and no traces of external spread after undergoing physical examination, he may receive either adjuvant radiotherapy of chemotherapy (Cancer Care Nova Scotia, 2005).
Management of Non-Seminoma Testicular Cancer:
This encompasses histological cancers of all subtypes and any pathological AFP elevation and ßhCG (Cancer Care Nova Scotia, 2005). The treatment options for managing this sort of testicular cancer involves various types of adjuvant chemotherapy and retroperitoneal lymph node dissection (Cancer Care Nova Scotia, 2005). Depending on the severity of the spread, a “nerve sparing” or “bilateral” retroperitoneal lymph node dissection might be recommended. However, Surveillance is recommended for both seminoma and non-seminoma testicular cancer types (Cancer Care Nova Scotia, 2005). In the case of the recurrent germ cell, the primary mode of treatment is chemotherapy (Cancer Care Nova Scotia, 2005). In some late relapse cases, surgery and radiotherapy may be required. Individualized treatment might be considered after an urgent clinical case conference has been held to determine what mode of treatment is best for a late relapse (Cancer Care Nova Scotia, 2005).
Ethical and legal issues associated with Testicular Cancer:
There is quite a hand full of legal and ethical issues that emanate from managing testicular cancer, however, the most stressed of all such issues is the issue fertility preservation. According to Robertson (2005), Cancer is a real life crisis for any cancer patient. Therefore, sometimes, fear of the unknown exerts an extra pressure to seek treatment at all cost. However, it is the legal and ethical responsibility of an oncologist to minimize the detrimental side effects that come along with the treatment of cancer in both younger and older patients (Robertson, 2005). Considering the fact that younger persons have a larger portion of their life ahead after they survive cancer, it is necessary to preserve their fertility along with their lives, while they undergo cancer treatment. Quite a substantial amount of people have been able to survive cancer, thanks to the help of the various innovative treatment methods available for the accomplishment of such goals. Cancer therapeutic treatments are capable of rendering a patient impotent/sterile after treatment, whereby causing oligospermia or azoospermia (American Society for Reproductive Medicine2, 2005).
Ethical Concerns
According to Robert (2005), not all oncologists are attentive towards preserving patient fertility during cancer treatments and therapeutic sessions. Whereas those involved with treating younger patients are very conscious of the applicable precautions necessary for preserving fertility. The lack of knowledge about whom/where to refer patients, particularly female cancer patient during treatment regarding fertility/sperm preservation makes it even more difficult to monitor the ethical aspects of patient fertility preservation. Although cryopreservation is an option for preserving fertility or sperm for matured males prior to cancer treatment, however not every cancer patient can afford sperm banking neither do health insurers cover the cost of sperm banking. As a result, some oncologist do not bother to inform their patients about fertility preservation through sperm banking. Another issue is the associated with the preservation of ovarian function when exposure of the ovaries to the hazards of chemotherapy and radiotherapy cannot be completely avoided during cancer treatment. Freezing oocytes can be encouraged but the success rate of fertilizing and giving birth to children from such eggs are really low compared to the rate of attempts worldwide. Other ethical issues surround helping cancer patients who lost their fertility during cancer management and treatment procedures and the harm that could be caused to their potential offspring as a result of genetic mutation and treatment effects. The fear is that if cancer patients desire to have children, they have a right to get the necessary support they need to accomplish such interests. However, their offspring may suffer physical defects, or turn out to become cancer patients in future due to high genetic mutation risk or other effects arising from the fertility preservation and pregnancy assistance processes. According to the American Society for Reproductive Medicine, 2013), It is necessary for cancer survivors who intend to become parents to conduct preimplantation genetic diagnosis in order to identify any risk associated with the birth of a child that would be at the risk of inheriting cancer.
Legal Issues
Legal and ethical norms demand that preserving fertility for minors who are not legally competent enough to consent to the procedure should be done to serve the best interest. Therefore, parents may be offered the opportunity to give their consent on behalf of minors on behalf of whom gonadal material (American Society for Reproductive Medicine, 2013). Studies used in this paper did not identify any legal or ethical analysis that concludes on any basis whatsoever that cancer survivors should not be given the necessary assistance/opportunity to reproduce.
Interprofessional Roles Associated with the management/treatment of Testicular Cancer
The main healthcare professionals involved in the treatment of testicular cancer are called oncologists. Oncologist administers different types of treatment approaches to cancer, in accordance with the appropriate treatment or the nature of cancer. Different oncologists are associated with different areas of cancer treatment specialty. The three main oncologist associated with the treatment of Testicular cancer are:
Radiation Oncologist: This refers to an oncologist who treats cancer patients with the aid of radiation therapy.
Surgical Oncologist: is an oncologist who treats cancer through surgery by removing abnormal tissue and /or tumor.
Medical Oncologist: is a medical specialist who treats cancer with the aid of chemotherapy, or targeted therapy and other types of medications (Cancer.net, 2015).
An oncology nurse: is medical practitioners (nurses) who care for individuals, families and patients or group of patients who have been diagnosed with cancer. Advance oncology nurse takes responsibility for managing major roles such as helping potential cancer risk patients to prevent cancer, cancer counseling, and medical oncologists with a chemotherapy administration among others. According to Ignatavicius et al., (2012) after the treatment of testicular cancer comes to an end, testicular cancer patients are likely to become sexually dysfunctional. For most men, who survive cancer and end up with sexual dysfunctionality, there is a change of life that initiates a psychological torment, especially for younger men. The fear of being sexually deficient, or being less sexually appealing is common among men who have been through cancer treatments. As a result, the fear of rejection causes a disruption in sexuality, which can have a significant effect on their self-esteem, confidence, ego and identity as a person. Men with such fears may suppress the feeling of sexual inadequacy and move on with their lives pretending to be fine rather than getting help. However, the burden of denial might end up placing their personal and work relationships under unnecessary strain. Therefore, as indicated previously, it is necessary to conduct an assessment of the testicular cancer survivor about his feelings and the aspects of his life where he needs support. Ignatavicious et al., (2012) recommended that friends, social groups, spiritual/religious groups, family, and community clubs can help patients with the psycho-social symptoms described above will be very helpful with getting the patient's mind off all the negative thoughts.
Providing Help for Effective Physical Condition Self-Management
Psycho-Emotional Health
Due to the emotional weight effect cancer usually has on family members such as spouses and the strains it imposes on the intimate part of such relationships, some couples end up gradually withdrawing from intimacy (Cancer Care Nova Scotia, 2005). In the case of younger men who have high hopes of fathering a child or children, being sexually involved with someone again and dating. It is usually psychologically daunting for some patients to think about how their life may change after or during testicular cancer treatment/management a patient's views and interest. Therefore, seeing a psychotherapists would be a very reasonable thing recommend to patients having sad and second thoughts (American Cancer Society, n.d.; Cancer Care Nova Scotia, 2005). Self-management after testicular treatment involves any form of extra decent support that a patient can get from cancer support groups, friend, family and any religious or spiritual group that can help elevate a patient' psychological status from away from depression (American Cancer Society, n.d.). In most cases, it is necessary to initiate a follow up care that would focus on exploring a patient's sexuality, intimacy, and relationship concerns; in order to ensure that everything is under proper control in the event of a situation whereby a patient experiences erectile dysfunction, visiting an urologist will be appropriate for determining the cause of the erectile dysfunction (Cancer Care Nova Scotia, 2005). Sometimes it could be as a result of psychological stress associated with cancer treatment.
Pathophysiology/Community-Based Care
If a patient undergoes surgery as the treatment in the form of open radical retroperitoneal lymph node dissection, he will be admitted for just one or two days after an MIS laparoscopy procedure (Ignatavicius & Workman, 2015). If there are no excessive wounds or any other medical complications, the patient will/should be discharged and sent to home without any dressing on the part where the incision has been made during the open orchiectomy (Ignatavicius & Workman, 2015). In most cases, a scrotal support is recommended to patients, in order to reduce the stress caused by the weight of the testicles on the scrotum until they can do without the scrotal support days later. For proper healing to take place, it is the duty of a nurse to make sure that a patient has adequate safety information for self-management once he returns home (Ignatavicius & Workman, 2015). Therefore, a nurse must ensure that the patient is aware of the following self-management safety precautions:
- The patient must not get involved in any form of physical stress or carry any item that weights beyond fifteen pounds;
- He must not drive a car for several weeks or climb stairs. He must have access to a toilet/bathroom facility on the floor where he resides and does not need to climb stairs (Ignatavicius & Workman, 2015).
- He may wear a dry dressing on the portion with the incision in order to prevent skin irritation on the stitched area when he moves around.
- The patient would need to visit the doctor again to check the healing process of the incision and for any other noticeable complications (Ignatavicius & Workman, 2015);
- The patient should be advice to carry out a self-examination at home and contact their doctors to book check-up appointments (Ignatavicius & Workman, 2015).
- He should also submit urine samples for serum level and tumor markers as well as for MRI and/or CT studies continuously for a minimum of three years;
- Patient would be able to take a shower within one to two days after laparoscopic orchiectomy as well as being able to return to his everyday activities (Ignatavicius & Workman, 2015);
- If a patient's testicular cancer requires repetitive surgery based on pathological observations and cancer stage, then he and his family must be informed about the situation.
If a man becomes completely sterile after testicular cancer treatment and sperm banking was not viable prior to the proceedings of the cancer treatment, he will need more information about his fertility or reproduction options (Ignatavicius & Workman, 2015). Therefore, such patients are usually referred to the American Fertility Society or the National Infertility Association. According to Martin et al., (2013) men who survived testicular cancer have been slightly ignored for too long neither have they themselves have not been speaking about the issue as often as they need to, so as to attract the right help in their direction. The proceedings of a workshop held for testicular cancer survivors indicated that there were a lot of issues such patients were willing to discuss but they did not know how, neither did they know whom to discuss the issues with. Therefore, more after-testicular-cancer self-management programs need to be established to reach out to the various needs of testicular cancer survivors. Self-management programs such as the workshop discussed by Martin et al., (2013) also provide an avenue for nurses to effectively provide information to testicular cancer survivor patients.
Conclusion
In conclusion, testicular cancer is a terminal life changing disease that brings about financial, psychological, social, and physical changes that can change the course of a person's life or that of their families. Nevertheless, testicular cancer survivors and their family would do better if they are provided with the right information and other resources they need to live through the dilemma associated with the new changes in their lives. Self-management is an essential part of recovery after cancer treatment is over with. However, some unforeseen complications may arise, patients should be aware of what to do, who to contact and how to go about their lives. The lack of adequate knowledge may escalate the psychological and physical needs of testicular cancer survivors to a detrimental state. Testicular cancer survivors can make the best of themselves after treatment through proper self-management.
Reference
American Cancer Society, (n.d.), Testicular Cancer, American Cancer Society; Retrieved from: http://www.cancer.org/acs/groups/cid/documents/webcontent/003142-pdf.pdf
American Society for Reproductive medicine2, (2005), Fertility Preservation and Reproduction in Cancer Patients, The Ethics Committee of the American Society for Reproductive Medicine, Fertility and Sterility (83)6, Elsevier Inc; Retrieved from: https://oncofertility.northwestern.edu/sites/oncofertility/files/legacy_files/asrm_ethics_report_on_fertility_preservation_and_reproduction_in_cancer_patients.pdf
American Society for Reproductive medicine1, (2005), Fertility Preservation and Reproduction in Patients Facing Gonadotoxic Therapies: A Committee Opinion, The Ethics Committee of the American Society for Reproductive Medicine, Fertility and Sterility (83)6, Elsevier Inc; Retrieved from:
Cancer Care Nova Scotia, (2005), Guidelines for the Management of Adult Testicular Cancer, Cancer Care Nova Scotia; Retrieved from: http://www.cancercare.ns.ca/site-cc/media/cancercare/TesticularGuidelinesREV2006(1)(1).pdf
Cancer.net, (2015), Types of Oncologists, Cancer.net; Retrieved from: http://www.cancer.net/navigating-cancer-care/cancer-basics/cancer-care-team/types-oncologists
Ignatavicius D. D., Winkelman, C., & Workman, M. L., (2012), Clinical Companion for Medical-Surgical Nursing: Patient-Centered Collaborative Care, Elsevier health sciences; retrieved from: https://books.google.com.ua/books?id=lFwCKRCwAGsC&pg=PT6332&lpg=PT6332&dq=testicular+cancer+self-management&source=bl&ots=w1jAQytZz-&sig=0d-E1L7hogtA7DOC-XLrBlY4iBY&hl=en&sa=X&ved=0ahUKEwiU5uPZvOjMAhXDiSwKHdopAUY4ChDoAQgzMAI#v=onepage&q=testicular%20cancer&f=false
Ignatavicius D. D., & Workman, M. L., (2015), Medical-Surgical Nursing: Patient-Centered Collaborative Care, Elsevier health sciences; retrieved from: https://books.google.com.ua/books?id=zdx2BgAAQBAJ&pg=PA1513&lpg=PA1513&dq=testicular+cancer+self-management&source=bl&ots=LKqNbs5Nv0&sig=84aYm5efRvmSeb1JAMNcsYF8pXQ&hl=en&sa=X&ved=0ahUKEwiU5uPZvOjMAhXDiSwKHdopAUY4ChDoAQgvMAE#v=onepage&q=testicular%20cancer%20self-management&f=false
Martin, F., Turner, A., Bourne, C., &Batehup, L., (2013), Development and Qualitative Evaluation of a Self-Management Workshop for Testicular Cancer Survivor–Initiated Follow-Up, Oncology Nursing Forum, 40(1); Retrieved from: http://www.ncsi.org.uk/wp-content/uploads/Development-and-Qualitative-Evaluation-of-a-Self-Man.pdf
Robertson, J. A., (2005), Cancer and fertility, Ethical and Legal Challenges, Journal of the National Cancer Institute Monograph, No. 34; Retrieved from: https://law.utexas.edu/faculty/jrobertson/cancerandfertility.pdf
Image = My Cat, Jack "The Lad"
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
What a load of bollocks!
Important issue, thanks for posting.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Thanks you! Please share..))
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
That check em graphic doe! XD
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
i love my balls, even though they get in the way sometimes and i sit on them.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
@jhip626 dude that is just hillarious.)))
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Very nice content.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
My friend, a kind reminder here.
#cn tag is stand for chinese.
However, no chinese was detected in this article.
Please use wisely for your tag,thank you.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Congratulations! This post has been upvoted from the communal account, @minnowsupport, by simeonburke from the Minnow Support Project. It's a witness project run by aggroed, ausbitbank, teamsteem, theprophet0, and someguy123. The goal is to help Steemit grow by supporting Minnows and creating a social network. Please find us in the Peace, Abundance, and Liberty Network (PALnet) Discord Channel. It's a completely public and open space to all members of the Steemit community who voluntarily choose to be there.
If you like what we're doing please upvote this comment so we can continue to build the community account that's supporting all members.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
great post keep going
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit