
Chronic Heart Failure | A Brief Review of the Pathophysiology
Heart failure is a common condition in the United States, especially in older adults. In fact, the lifetime risk of developing heart failure if you’re an American over the age of 40 years of age is great than 20%. Just think about that statistic for one second. Nearly, 1/5 of American over the age of 40 are at risk of developing heart failure. If that isn’t scary enough, the mortality rate is roughly 50% within 5 years despite recent advancements in medicine.
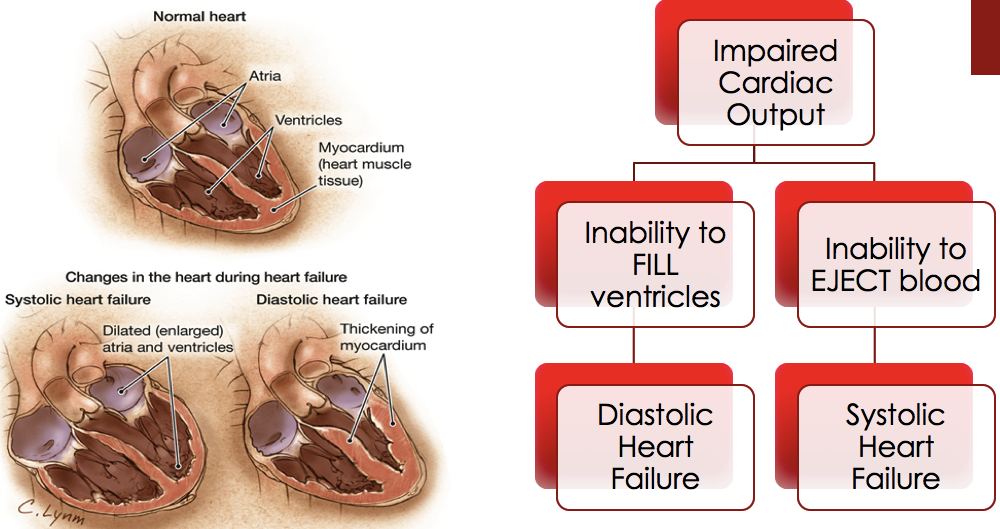
Heart failure occurs when the heart is not able to supply sufficient oxygen-rich blood to the body, because of impaired ability of the ventricle to either fill or eject blood. Heart failure is commonly classified as either ischemic (due to a decrease in blood supply, such as from a myocardial infarction) or non-ischemic, such as from long-standing uncontrolled hypertension. Other less common causes of heart failure include valvular disease, excessive alcohol intake, or illicit drug use, congenital heart defects, viral infections, diabetes, and cardiotoxic drugs.
Symptoms of Heart Failure can occur due to problems with systolic (contraction) or diastolic (relaxation) functions of the heart. Patients with heart failure usually cycle through periods of stability and exacerbation (increase in frequency of symptoms). Exacerbations frequently result in hospitalizations and negatively impact the patient’s quality of life.

An ultrasound of the heart (referred to commonly as an echocardiography or ECHO) provides useful information when heart failure is suspected, including an estimated of the left ventricular ejection fraction (LVEF). The left ventricular ejection fraction is a measurement of how much blood is pumped out of the left ventricle (the main pumping chamber of the heart) with each contraction. An ejection fraction less than 40% indicates systolic dysfunction or heart failure with a reduced ejection fraction (HrEF). This type of heart failure is the most widely studied.
Another type of heart failure is heart failure with an ejection fraction great than 50% which is referred to as heart failure with preserved ejection fraction (HFpEF). This type of heart failure is much less commonly studied and reported in the literature. For this reason, many of the drugs used to treat heart failure have been studied and thus meant to treat patients with HFrEF. Treatments in patients with heart failure preserved ejection fraction (HFpEF) often are aimed to treat the other underlying comorbidities (or disease states) which are contributing to the heart failure.
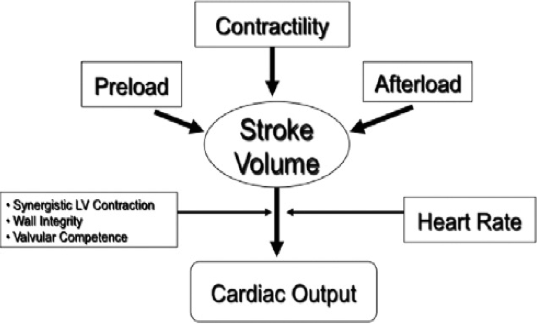
The cardiac output (CO) is the volume of blood that is pumped by the heart in one minute. Cardiac output is a function of the heart rate (HR) and the stroke volume (SV), or the volume of blood ejected from the left ventricle during one complete heart beat (cardiac cycle). The stroke volume also depends on the preload, afterload, and contractility of the heart. The cardiac index (CI) relates the cardiac output to the size of the patient, and is calculated by dividing the cardiac output by the body surface area (BSA).
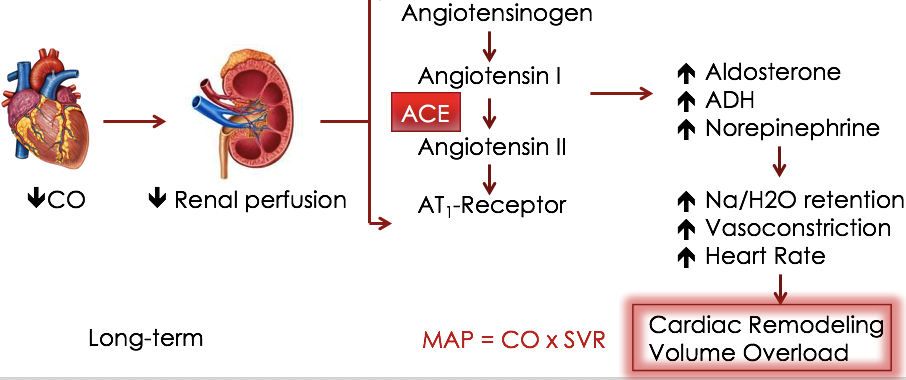
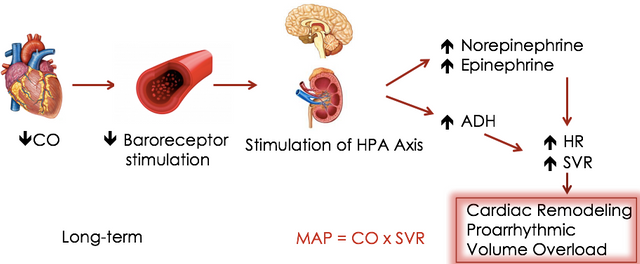
During low cardiac output states (for instance patients with heart failure); neurohormones are released that increase the blood volume or increase the force or speed of contractions. These compensatory mechanisms temporarily increase the cardiac output, but over time will further compromise the heart. Chronic neurohormonal activation increases the workload of the heart which causes damage to the myocytes and produces changes in the size, composition and shape of the heart. This is commonly referred to as cardiac remodeling.
There are two main neurohormonal pathways activated in heart failure. The first pathway in the renin angiotensin aldosterone system (referred to as RAAS). In this pathway, angiotensinogen in split by renin into angiotensin I. Angiotensin I is further converted into angiotensin II by the angiotensin-converting enzyme (ACE). Angiotensin II causes blood vessel constriction (referred to commonly as vasoconstriction), and stimulates the release of aldosterone (from the adrenal glands) and vasopressin from the pituitary glands. Aldosterone causes sodium and water retention, and increases potassium excretion. In addition, vasopression also causes vasoconstriction and water retention. Although in the short term, these compensatory mechanisms can help to increase the cardiac output and be beneficial. The long term consequences are much more severe and lead to cardiac remodeling and further damage to the heart, which further exacerbates heart failure.
Activation of the second pathway, the sympathetic nervous system (commonly referred to as the SNS), results in the release of norepinephrine (NE) and epinephrine (EPI). These catecholamines cause an increase in heart rate, contractility (positive inotropy) and vasoconstriction). Like the RAAS system, this system also produces an increase in cardiac output, which helps in the short-term. However, just like the RAAS system, the long term consequences are much more severe and lead to cardiac remodeling and further damage to the heart, which further exacerbates heart failure.
@originalworks
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
The @OriginalWorks bot has determined this post by @tspink to be original material and upvoted it!
To call @OriginalWorks, simply reply to any post with @originalworks or !originalworks in your message!
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Upvoted and shared! Thanks for putting the research into this and sharing it @tspink! You're intro is really good, we often like to think of statistics as just that, a number which doesn't affect us. It's not until we become one of those statistics that things hit us!
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Thank you for the continued support @pv-p I agree, I often fall victim to this kind of thinking myself. Not until you stop to think about how many people it affects overall that it really starts to stand out.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit