Telecare is to healthcare what ecommerce is to retail. Telecare is bringing a new model of internet enabled healthcare services which is obliterating the traditional model of doctor-patient relationships. It is cutting the brick & mortar hospitals out by creating a direct connect platform between patients and providers. Telecare enabled kiosks (manned/unmanned) are emerging as a real choice for people who want immediate attention.
Smart devices and wearables are transforming monitoring and management of patients. Voice integration with home pod like devices is accelerating the promise of a simpler universal healthcare interconnect. Homecare is bringing even the ICU home and transforming geriatric care. Patient care is becoming a data scientist’s game with analytics driving decisions and AI automating rapid response systems.
So does this mean that Telecare is going to completely disrupt healthcare just like Amazon is doing? Will it give us many choices in terms of basic healthcare services? Will it allow any patient to visit any hospital and still get the same level of service? Can healthcare become a utility service that is delivered to you irrespective of your physical location? Finally will we all have healthcare that is affordable, personalized and reliable?
If you said yes, you would be WRONG!
Here are some quick definitions that will help us understand the landscape better:
- Telemedicine: Remote intervention by a doctor or other specialist
- Telehealth: Remote monitoring solution with connected devices
- Telecare: Ecosystem of patients, providers and devices for a fully managed healthcare solution
There are many reasons that Telecare has been a disappointment so far and it has miles to go before we can call it mainstream. Did you know that the first telehealth commercial solution came out almost 40 years ago? But today telecare is still struggling to put together a cohesive revenue/delivery model that will justify costs and provide quality of care.
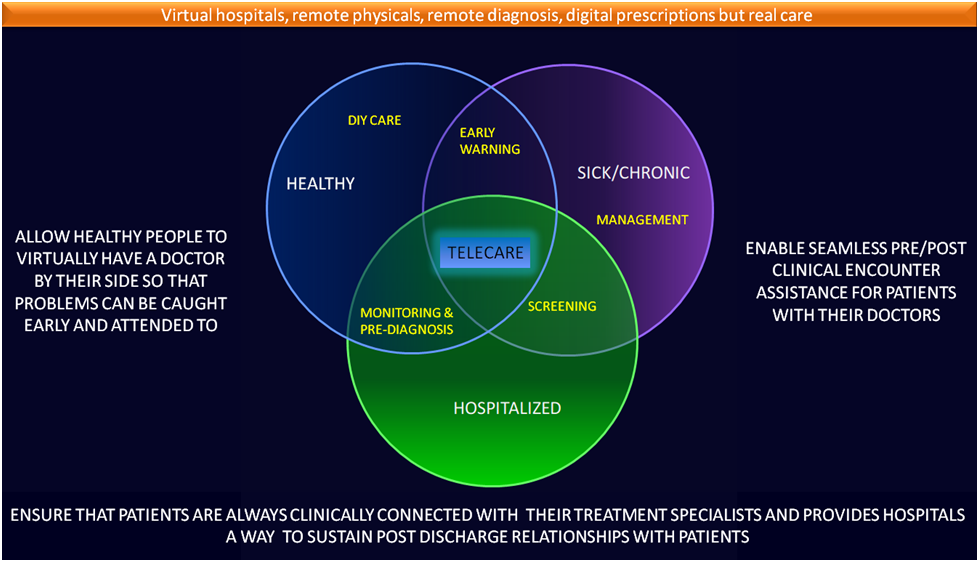
Let us dive into the spectrum of healthcare interactions which will serve as a foundation for conclusions that we will draw.
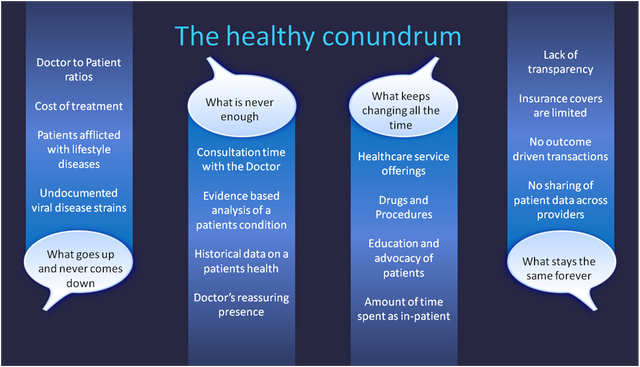
The key takeaway here is that there are some problems that can be never fixed (at least currently). AI is attempting to tackle the doctor to patient ratio imbalances. Our inactivity is increasing the advent of lifestyle diseases. Patient data sharing is a gargantuan exercise and today consists mainly of passing the buck from one provider to the other.
Costs are another matter altogether. The pharmaceutical industry has shown itself as being impervious to economic downturns. Insurance companies are interested only in reducing their payouts. Hospitals try to maximize inpatient revenue. Independent providers rely on captive patient groups to sustain their practice.
Transparency seems to be a goal that can never be attained by healthcare. The lack of clarity into clinical decisions is just the tip of the iceberg. There are no audits since all encounters are transactional in nature. Once a patient walks away, the record of treatment hardly matters unless there is a legal deposition. This means that quality procedures and protocols are predictably missing from standard healthcare fare
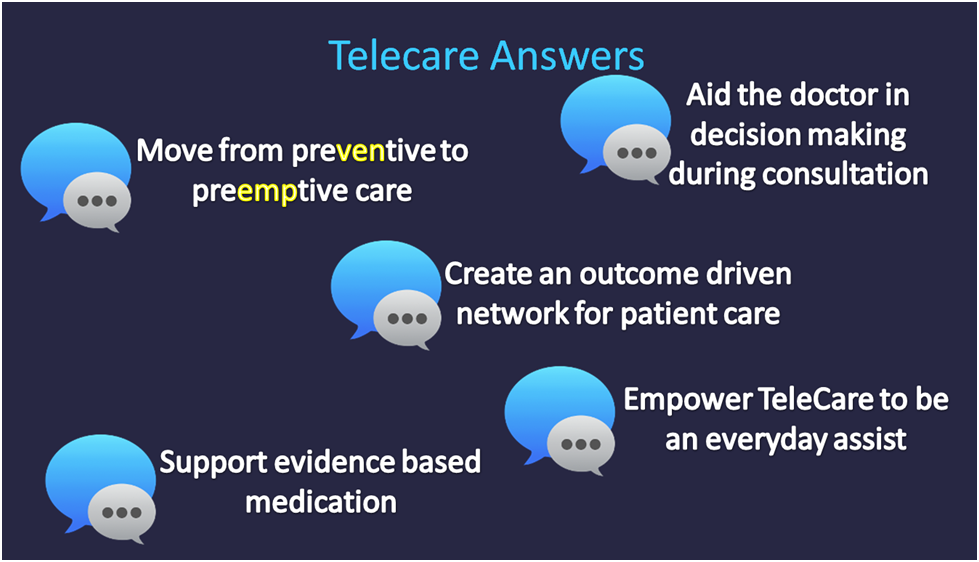
Telecare evolved as a solution to many of healthcare’s problems. A patient visit to the doctor typically signifies that there is an existing problem which was left unattended for a longer time than desired. So if the doctor could be involved with the patient before the doctor-patient encounter then it is quite possible that either the problem is caught early on or timely remedies may palliate the problem before hand.
Telecare works best when a network of related providers is involved so that the patient’s experience is seamless and it becomes outcome driven. It also needs data to be analyzed, summarized and presented so that the provider can take accurate decisions.
Healthcare is a community driven program. The community in this case is built on references and experiences of other patients as well as providers. There is also a hidden revenue sharing protocol which largely determines available choices. References are the backbone of the network thus determining initial provider selection, sustenance of trust and repudiation of alternative choices. The biggest bane of Telecare has been the complete absence of digital prescriptions unless the prescriber is already associated with the retail pharmacy. Without remote prescriptions, Telecare is toothless
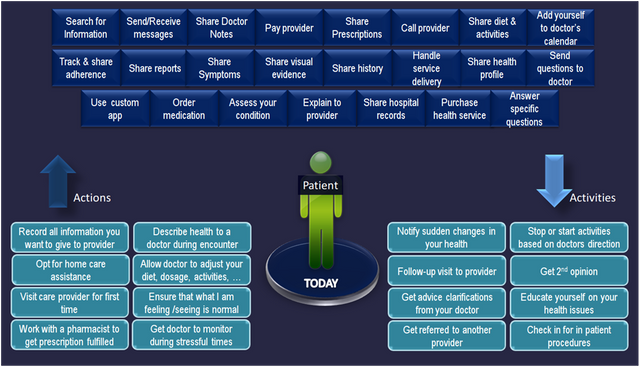
When we consider the view from the patient it is a combination of activities that the patient carries out habitually (like book keeping), complemented by demonstrable outcomes (actions). On a telecare platform patients and providers must work together to maintain a consistent state across all interactions.
There are multiple information sources, more than one interaction channel and probably a set of diverse apps. There is a heterogeneous mix of providers who offer care, consumables, point services and advocacy. There are also various health record sources that make it very complex from hardcopies of reports to online PACS data viewing services.
What jumps out at you is the tight knit circle of providers with whom the patient has to interact with in order to achieve his objectives. Diagnostic labs, primary care clinics, kiosks, pharmacies, hospitals and point service providers have to collaborate together to provide a seamless experience to the patient. If you throw insurance into the mix then it becomes clear that navigating healthcare is like being stuck in downtown traffic.
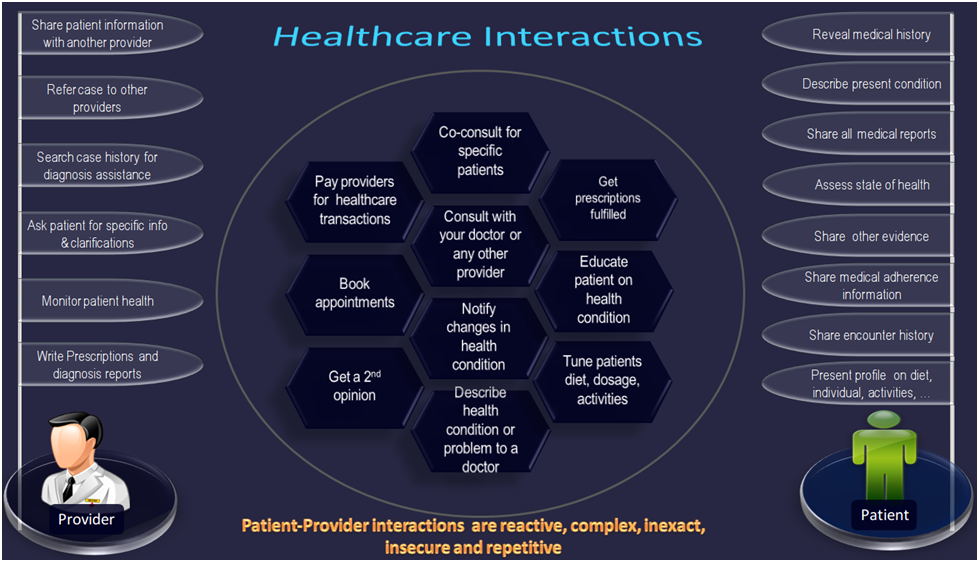
When we look at the nature of the interaction between the provider and the patient, we are struck by the insane amount of repetitive dialogue that occurs during every encounter. Basic questions will be asked, information gleaned and decisions taken. This duplication of effort is bi-directional and is an unintended consequence of the on-demand nature of providers reacting to patient’s problems.
During every encounter, the provider must first scan the patient’s past records, dredge his memory for personalized information regarding the patient and also rely on historical information across multiple providers to make decisions that are not arbitrary.
Part of the problem is the severe lack of trust within the system. Providers are inherently careful about making mistakes due to erroneous conclusions drawn by other providers. Hence every document is scrutinized for the nth possible time. Every decision made is second guessed. Past clinical procedures are dissected, questioned and sometimes even negated by other compensatory treatments. The system works avidly on reference points and provider chains that try and cover up the problem of trust deficits.
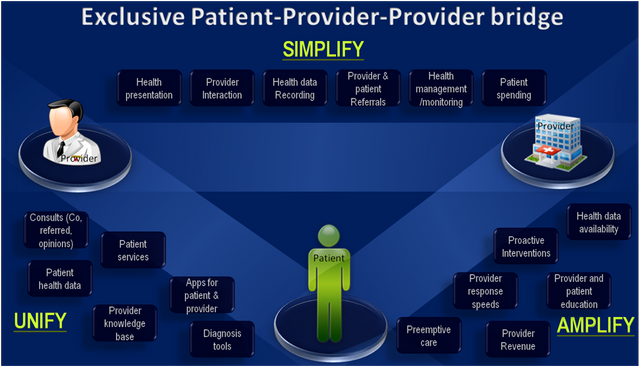
Telecare’s role in welding an ecosystem together cannot be insignificant. It is a prime mover in putting together a common platform upon which every participant can collaborate, monitor, measure and improve outcomes. All patient services must be able to draw from a common pool of data. Interactions need to be fast, accurate and relevant. In addition the provider must not spend inordinate amount of time sifting through piles of data to arrive at decisions.
When IOT enters the mix then this situation is infinitely more complex. Someone has to weed out irrelevant data. Tools have to constantly prune decision trees (sometimes in real time) in order to facilitate on demand care for patients. Consider a heart rate monitor emitting one reading per minute with a variety of positive/negative spikes in reaction to hundreds of stimuli. You end up with a daily requirement to scan and prune around 1500 different readings in a conservative home care data collection scenario.
Healthcare is stuck in a time warp as far as openness and speed of response is considered. In fact time is relatively of little meaning to a provider because of the skewed provider to patient ratio. In order to bring everyone together on a common decision making process, it is a colossal task indeed to get everyone on the same platform. In many situations especially where large hospitals are involved it is well nigh impossible because of the differences in deployed software. In addition there is no incentive driven mechanism to accomplish instant sharing and open collaboration.
This is the eternal promise that telecare holds which in my infinite wisdom has not happened yet! The traditional model visiting doctors is passé. Each patient has to learn to independently care for himself/herself with some amount of remote help. The assistance could be from a specialist or a primary doctor. Data is the driver here and there will be oodles of it as consumer wearables mix with home care appliances. Telecare has been setup for this precise approach for decades and it is a pity that it has not come to roost yet. In the future health monitoring has to be self driven unless you absolutely need an independent care partner. This means that we must be able to understand our own symptoms and/or device readings to an extent that helps us to preemptively interact with a provider before the situation gets out of hand. It is also critical that the exact opposite must hold true as well with the provider alerting the patient proactively regarding potential health problems that need addressing.
This in essence the central problem that blockchain will solve. There must be motivation from different providers to share their data about a specific patient. There must also be a solid financial reason to continue storing historical records beyond pulling it up for reference purposes. There must be an integrated financial model that will allow money to be distributed across providers as part of a single patient facing transaction.
The inflection point is NOW
- Healthcare needs a single currency system to unify and remove the stop-go nature of patient handling in the system. Blockchain can create a universal healthcare coin that will work across the country (if not the globe) which will unify insurance providers, providers and even concierge services on an efficient care delivery network
- In order to bridge the patient-provider gap, a systematic scalable referral mechanism needs to be tightly coupled with normal functioning. Part of the money in the system will be used to create a referral marketing system between patients making every patient an investor in another patients well being
- This is a great opportunity to legalize money flowing around between pharmaceutical companies, providers, device manufacturers and brokers. Since this cost is integrated into the existing system already it will be easy for blockchain to give it an aura of acceptability and avoid questionable accounting practices
- Data sharing is going to be a boon with blockchain implementations as the system will build a data sharing fee directly to all transactions. This fee will universalize the acceptability of records submitted by a decentralized provider ecosystem. Different types of contracts will determine the usage, frequency of access and access method
- Collaborative decision making needs to be enabled by on demand transactions, which is possible only when enforceable contracts exist. Triages on demand will be a fruitful byproduct of the smart contract ledger model which will reassure the patient instantly with 2nd opinions as well as co-consults
- A virtual hospital which is a conglomeration of decentralized providers and disconnected patients is a great example for what blockchain can achieve by just being itself. Concierge services which facilitate patient transfers, patient engagement services and advocacy can be pre built into the system at very reasonable rates
- Insurance claims are a bone of contention which can be fixed easily with contract based payouts. Transparent payouts are going to reduce the constant triaging between patient, provider and insurance representatives
- Proactive or preemptive care is a dream of healthcare today that can be instantly converted into reality by employing smart contracts that determine cost, frequency and period of such care. It will incentivize wearable manufacturers to share curated data, reward expert analysis and compensate point of care professionals
- Maybe blockchain’s biggest boon is the reintegration of primary healthcare. By clearly definining roles for general physicians and providing them with a transparent revenue sharing platform, it brings the general physician to the forefront of all clinical interactions
- Affordability is a byproduct of transparency. When costs are universally available then affordability becomes a routine matter. When services can be compared and fixed contracts control spending then blockchain will achieve the most emphatic benefit that can accrue to a patient. Transparency will also bring higher volumes because the trust factor is reasserted in the system and hence providers are happy as well
- Blockchain can completely revolutionize the prescription system. It can make digital prescriptions legal in a court of law. Illegal prescription refills can be invalidated. Prescription reuse can be stopped in its tracks. It can completely void the nexus between providers and pharmacies and that would be phenomenal. It will completely authenticate Telicare as a healthcare delivery model
Healthcare has been plagued with ills for as long as we can remember. The diseases that healthcare has been suffering with are rising costs, lack of transparency, inefficient care, easy access to expert providers and operational road blocks. Healthcare needs a new engine and blockchain backed Telecare is the perfect fit. Blockchain is the spine that healthcare needs and it is time that providers around the world join together to deliver their most significant baby yet.