Anemia is one of the most prevalent hematological disorders in the world, which primarily hinders the transport of oxygen. This obstruction occurs either due to abnormalities in red blood cells or in the hemoglobin present in them, which are the oxygen transporters. As a medical student, this year I completed my medicine ward rotations, and I encountered various forms of anemia both through my studies and clinical settings. There wasn’t a single day in the medicine ward where I didn’t come across an anemic patient. In third-world countries, anemia is so common that the criteria for anemia itself has been lowered. According to one study, the normal hemoglobin levels in Asian women are quite low, which is why the criteria for anemia has been significantly reduced for them [1].
Our university runs a large NGO called the Patient Welfare Association (PWA), which is not only one of the largest non-governmental organizations in Pakistan but also in all of Asia. It donates thousands of liters of blood to those in need every year. It provides free assistance to innocent children suffering from diseases like thalassemia and sickle cell anemia. Such campaigns are continuously held at our university, and people donate blood in the thousands.
Anyways, in this post, I will break down the key aspects of different morphological forms of anemia and address the given case study, providing a very detailed explanation from a medical perspective.

 |  |
|---|
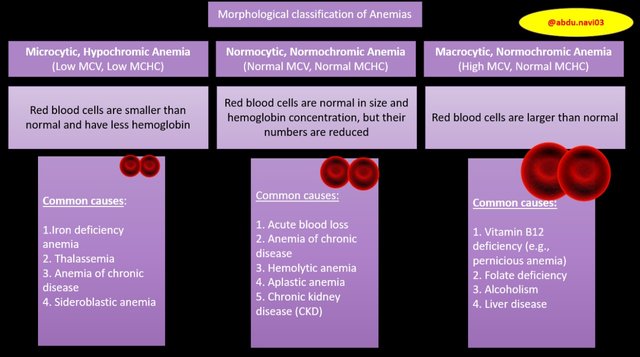
Anemia can be classified on many basis, like morphological classification (based upon RBCs size and hemoglobin content), etiological classification (depends upon underlying cause), pathophysiological classification (explained later), classification based upon severity or blood smear picture.
In this module, we are specifically concerned about morphological classification.
The mean corpuscular volume (MCV) is used to determine the average size of RBCs, The normal size of red blood cells is 80-100 fl (femtolitre) with biconcave shape, this shape allows the maximum exchange of gases (o2 and co2) through them. Morphologically Anemias can be distinguished based upon the MCV values. These values can either be normal means 80-100fl leading to Normocytic Anemia, lower MCV <80fl leading to Microcytic Anemia and >100fl leading to Macrocytic Anemia.
1)Microcytic Anemia (micro= small, cyte=cell, anemia= low hb level)
You can easily distinguish Microcytic anemia by the presence of red blood cells that are smaller than the normal size, specifically with MCV of <80 femtoliters. This type of anemia is often associated with inadequate hemoglobin synthesis relative to the size of the RBCs, like in iron deficiencies.
2) Normocytic Anemia (normo= normal, cyte=cell, anemia= low hb level)
However, Normocytic anemia is characterized by red blood cells that are of normal size, with an MCV ranging from 80 to 100 fL. This type of anemia occur when the body’s production of RBCs may not adequately compensate for losses like in acute blood loss, anemia of chronic disease, and renal failure,
3) Macrocytic Anemia (macro= large, cyte=cell, anemia= low hb level)
Lastly, Macrocytic anemia is the easiest one to pick on blood tests reports as it is characterized by the presence of red blood cells that are larger than normal, typically with an MCV >100 fL This type of anemia occurs when there’s impaired DNA synthesis leads to the production of larger, immature RBCs, like in vitamin B12 deficiency and folate deficieny.
Have you ever had anemia? Attach evidence. If you’ve had anemia, provide a brief explanation or evidence (like lab results or a story). If you haven’t, share an anemia case of a friend, relative, or acquaintance (while keeping their identity confidential).
I have never gotten anemia uptil now but I can surely share a case that I encountered during my clinical rotations, 2 months back when I was posted in Medicine ward, a 7-year-old boy was brought to the OPD with complaints of persistent fatigue, progressive pallor, and recurrent upper respiratory infections over the past four months leading to weight loss. According to parents he is tired all the times with episodes of dizziness and headaches, shortness of breath during play and a decreased appetite.
When I did physical examination of him, he appeared thin and pale with mild frontal bossing, with an increased heart rate (tachycardia) and a respiratory rate of 22 breaths per minute. His blood pressure was low, and his growth is slightly delayed for his age. Pale conjunctivae and mild scleral icterus (yellow eyes) were noted by me. Abdominal examination showed splenomegaly (enlarged spleen) and mild hepatomegaly (enlarged liver).
To establish the diagnosis, laboratory tests were performed:
| Test | Value | Reference Range | Remarks |
|---|---|---|---|
| Hemoglobin | 7.2 g/dL | 11.5 - 15.5 g/dL | Severe Anemia |
| Mean Corpuscular Volume (MCV) | 68 fL | 80 - 95 fL | Microcytic Anemia |
| Red Blood Cell Count (RBC) | Elevated | 4.0 - 5.2 million/µL | |
| Reticulocyte Count | Elevated | 0.5 - 2.5% | Increased red blood cell turnover |
| Serum Iron | Normal | 50 - 170 µg/dL | No Iron Deficiency Anemia |
| Total Iron Binding Capacity (TIBC) | Normal | 240 - 450 µg/dL | |
| Ferritin | Normal | 12 - 300 ng/mL | |
| Hemoglobin F | Elevated | <1% | Suggestive of Thalassemia |
| Hemoglobin A2 | Elevated | <3.5% | Suggestive of Thalassemia |
| Bilirubin (Total) | Mildly elevated | 0.1 - 1.2 mg/dL | |
| Peripheral Blood Smear | Hypochromic microcytic cells, target cells, basophilic stippling, and nucleated red blood cells | Thalassemia |
Given the severity of the anemia, the boy was initially managed with packed red blood cell transfusions to correct the hemoglobin deficiency. For long-term management, regular blood transfusions every 3 to 4 weeks were planned to maintain appropriate hemoglobin levels. To prevent iron overload from the transfusions, iron chelation therapy with deferoxamine was initiated. The boy will continue to visit the ward regularly for monitoring and treatment. I pray for his swift recovery and hope he gains strength soon.
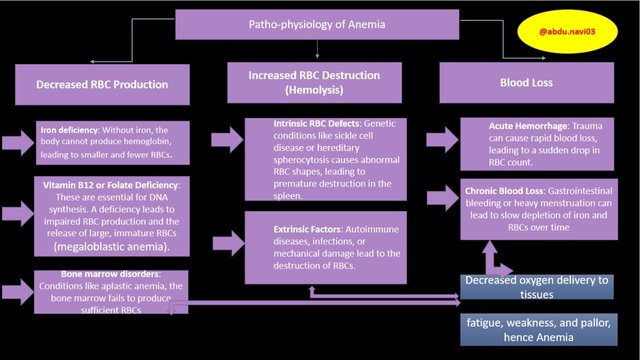
So if we explain the pathophysiology of anemia, the whole issue revolves around the body's unmatched oxygen demand.
What happens is that inside our red blood cells (RBCs) there is hemoglobin, which binds with oxygen when it reaches the lungs, and then, through blood circulation, it supplies oxygen to all the tissues in the body that need it. As I mentioned in my previous post, our body respires aerobically, and every tissue needs oxygen to stay alive and function properly. So, if hemoglobin decreases or if the RBCs become abnormal, the oxygen-carrying capacity of the RBCs, i.e., hemoglobin, is impaired, which deprives tissues of oxygen.
Because of this, the body activates certain compensatory mechanisms. For example, our heart rate increases so that the blood, which has less hemoglobin, may circulate rapidly throughout the body in an attempt to meet the body's oxygen demand. However, prolonged oxygen deprivation to the tissues can cause symptoms such as fatigue and weakness (due to reduced blood supply to the muscles, causing constant tiredness).
Our body and skin may appear pale because the blood supply decreases, leading to less visible redness, which is most noticeable on the skin, lips, and other mucocutaneous areas.
Anemia can also cause shortness of breath (dyspnea) because low oxygen levels in the blood make breathing more difficult, especially during physical activities, as the body tries to compensate by increasing the respiratory rate. Normally, circulating blood keeps our body warm, but in anemic conditions, inadequate oxygenation affects circulation, particularly in the extremities, leading to a sensation of coldness. Additionally, it can cause headaches and difficulty concentrating because reduced oxygen supply to the brain impairs cognitive function and mental concentration within seconds of blood deprivation, as the brain is one of the most oxygen-dependent organs in the body.
Laboratory Results of Given Case
| Test | Result | Normal Range (approx.) | Interpretation |
|---|---|---|---|
| Hemoglobin | 9 g/dL | 12-16 g/dL (women) | Low (Anemia) |
| MCV | 71 fL | 80-100 fL | Low (Microcytic Anemia) |
| HCM | 24 pg | 27-31 pg | Low (Hypochromic) |
| CHCM | 27 g/L | 32-36 g/L | Low (Hypochromic) |
| HCG | Positive | - | Suggestive of Pregnancy |
So based on the lab reports, the patient exhibits microcytic hypochromic anemia. The most common cause of microcytic hypochromic anemia is iron deficiency anemia, and in third-world countries, beta thalassemia is also a major cause. Given that the patient in the case report is pregnant and there are no obvious signs or findings of beta thalassemia mentioned, iron deficiency anemia is very likely due to increased demands during pregnancy. The very first medication we ask pregnant patients if they took during their pregnancy are folate and iron tablets. That’s because pregnant women require some additional iron to support fetal development and also to compensate for the increased plasma volume that occurs during pregnancy. Normally, women are more prone to anemia as they lose some blood monthly because of menstruation. So iron tablets are a necessity during pregnancy. Without adequate iron intake or supplementation, hemoglobin synthesis is impaired, leading to smaller and paler RBCs, as reflected by the lab reports which show low MCV and low MCHC values.
The fainting and pallor observed in this patient are very common and classical symptoms of anemia. As I have already explained, even a few seconds of hypoxia to the brain can cause dizziness and fainting, so a constant reduced oxygen supply to the brain can cause cognitive impairment (decline in mental abilities such as memory, attention, and problem-solving in daily functioning) and fainting. Pallor results from reduced oxygenation of the tissues, particularly the skin, lips, fingers, and mucous membranes. It is crucial for the patient to receive iron supplementation to prevent further complications during pregnancy, such as low birth weight or even preterm delivery.
Reference;
[1] Varghese, Jithin Sam, Tinku Thomas and Anura V. Kurpad. “Evaluation of haemoglobin cut-off for mild anaemia in Asians - analysis of multiple rounds of two national nutrition surveys.” The Indian Journal of Medical Research 150 (2019): 385 - 389.
Thank you, @dexsyluz and @aaliarubab, for organizing this medical sciences contest and giving me the opportunity to present my knowledge and understanding. I truly appreciate it!
Regards,
Dr @abdu.navi03
Once again, brilliant explanation from you. A lot of my friends have anemia specially the females. Why do you think that's the case?
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Thank you so much for your thoughtful question! You're absolutely right—anemia, especially iron deficiency anemia, is much more common in women. One of the main reasons is the monthly menstrual cycle, which naturally causes iron loss. Pregnancy also increases the body's demand for iron and folate, and if this isn't balanced with proper intake, it can lead to deficiencies. In countries with lower socioeconomic conditions, poor nutrition, particularly in young women, adds to the risk. So it's really important to focus on a balanced diet and proper supplementation to prevent these issues
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit