Antibiotic resistance is a result of the overuse and misuse of antibiotics in the medical community. Furthermore, antibiotics that are spontaneously incorporated into the environment exacerbate the problem.
Antibiotics, which are used to treat bacterial infections, have saved the lives of millions of people around the world since they were discovered. Resistance to antibiotics is a severe problem that has arisen as a result of the overuse and misapplication of antibiotics. Furthermore, antibiotics that are spontaneously incorporated into the environment exacerbate the problem.

Source
Antibiotics can wind up in the soil and water because leftover antibiotics are thrown away or because certain antibiotics consumed by people are flushed out of the body without being metabolized. The intake of antibiotics by humans, on the other hand, is not the primary source of antibiotic contamination in the environment. Antibiotics are also used in pesticides and the treatment of animal ailments, in addition to their other applications.
In industrial processes, such as the mixing of antibiotics from crops and grasslands into waterways, mixing of antibiotic-containing waste products used by humans and pets into sewers, and the production of ethanol, the formation of antibiotic-containing end products occurs. These industrial processes, as well as other factors, are the most significant sources of antibiotic-related pollution.
What Is Antibiotic Resistance and How Does It Affect Us? Which Antibiotics Have the Most Negative Impact on the Environment?

SourceAntibiotic resistance linked to soil pollution
So, what is the process by which antibiotic resistance develops? The abuse of antibiotics, as well as the wrong selection of the most appropriate antibiotic for the ailment, are the two most significant contributors to this situation. In 2015, the Center for Disease Dynamics, Economics, and Policy (CDDEP) published the 2021 World Antibiotics Report, which found that global antibiotic usage increased by 65 percent between 2000 and 2015. If nothing is done, it is predicted that antibiotic consumption will increase by 200 percent by 2030. It is expected that the use of animal antibiotics will increase by 11.5 percent between 2017 and 2030.
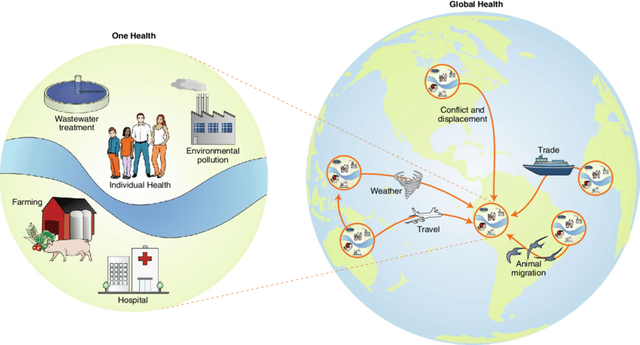
So, what is it about antibiotic resistance that makes it such a global concern? It is possible that bacterial infections that are today considered "simple" would no longer be treated in the coming years, according to the World Health Organization. According to another study, infections caused by bacteria that are resistant to antibiotics are anticipated to account for more fatalities by 2050 than cancer and diabetes combined in the future.
What measures are being done to prevent antibiotic contamination?
SourceDefining and combating antibiotic resistance
Antibiotic resistance can be prevented by taking steps, both individually and collectively, to avoid the spread of antibiotic resistance.
The first and most important thing is that we should not strive to protect ourselves from infections that require antibacterial therapy. In order to accomplish this, we should wash our hands frequently, maintain proper hygiene when preparing meals, and avoid close contact with sick individuals. As a result, when we use antibiotics, we reduce the likelihood of resistance developing. Antibiotics should only be taken if they have been prescribed and approved by a medical professional. Other people should never be given antibiotics, and we should never insist that our doctor prescribe antibiotics for our own health problems.

SourceAntimicrobial Resistance in Rivers
With the passage of time, antibiotic resistance develops. However, since the use of antibiotics continues to rise on a daily basis, the problem is becoming more widespread and posing a threat to global health. It is possible to slow the spread of antibiotic-resistant bacteria by taking the following procedures.
Reference: