![Screenshot_20211017-210828_Canva[1].jpg](https://steemitimages.com/640x0/https://cdn.steemitimages.com/DQmbiqkZxH26spc1VcxRpqNBJYaR72eYeRVfoGuj4ecp7bF/Screenshot_20211017-210828_Canva[1].jpg) Image Made With Canva App
Image Made With Canva App

INTRODUCTION
Hello Everyone
Hello Campusconnect Family
It's Dr. @kingmyke here and I am coming to you all with a new initiative, the KingMyke Lecture Series. I am an enthusiastic Medical student at the University Of Nigeria, Enugu Campus and I want to drop a thing or two about what I have learnt so far during my journey in Medical School.
Enjoy!!!

DEFINITION
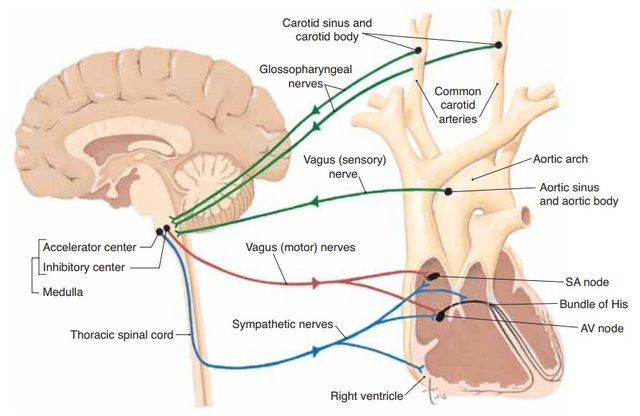
Heart rate is the number of times the heart beats per minute. Basic heart rate is set by the intrinsic conducting system particularly the SA node. This rate is modified by the autonomic nervous system. Stimulation of the sympathetic increases the rate (chronotropy) and force (inotropy) of contraction and parasympathetic stimulation slows the heart. The heart is under tonic inhibition from the vagus nerve which predominates over the excitation from the sympathetic nerve. Both systems work in a reciprocal relationship; an increase in sympathetic stimulation is accompanied by a decrease in vagal inhibition and vice versa.
Sympathetic and parasympathetic discharge to the heart is however under the control of groups of neurons in the medulla called the cardiac center.
This consists of:
The cardio inhibitory area located in the dorsal nucleus of the vagus and the nucleus ambiguous sends parasympathetic nerves via the vagus to the heart,
The cardio accelerator area projects to sympathetic neurons in the T1 – T5 levels of the spinal cord. These preganglionic neurons synapse with ganglionic neurons in the upper thoracic sympathetic trunk.
Sensory area located in the nucleus tractus solitarius
The heart is exhibits a Vagal tone. Cutting the vagus increases the HR from 70 – 75/min to 100 – 120/min.

REGULATION OF HEART RATE
1. HIGHER CENTERS:
Centers in the cerebral cortex (limbic cortex) via the hypothalamus stimulate the cardiac center and affect heart rate. Specific factors include; excitement, anger fear and sexual arousal increase HR. Depression and grief can decrease HR.
2. RESPIRATORY CENTERS:
During inspiration respiratory centers in medulla radiate impulses to cardiac center causing an increase in HR. /.During expiration HR falls. This phenomenon is known as sinus arrhythmia.
3. CHEMORECEPTORS:
Stimulation of chemoreceptors (aortic and carotid bodies) by rise in pco2 and hydrogen ion concentration not only feeds back impulses to respiratory centers in medulla but also exerts influence on vasomotor and cardiac center. This results in peripheral vasoconstriction and bradycardia. Hypoxia however causes hyperpnea and increased secretion of catecholamines from adrenal glands resulting in tachycardia.
4. BARORECEPTORS:
When stimulated the baroreceptors send their impulses via the vagus and glossopharyngeal nerves to the nucleus tractus solitarius which sends inhibitory impulses to the cardio accelerator area and vaso constrictor nerves but excites vagal innervation to the heart. This results in a slowing of heart rate, vasodilation and fall in blood pressure.
5. ATRIAL RECEPTORS:
. Stimulation of type B atrial stretch receptors leads to an increase in heart rate. Type B atrial stretch receptors discharge in late diastole at peak of atrial filling.
. The type A receptors discharge during atrial systole . Rapid infusion of blood or saline sometimes increases heart rate if it was initially low. This is known as the Bainbridge reflex. It is mediated by atrial stretch receptors via the vagus (vagal inhibition and sympathetic facilitation). It is abolished by vagotomy. The reflex competes with baroreceptor mediated decrease in heart rate produced by volume expansion.
6. HYPOXIA AND HYPERCAPNIA:
These have a direct effect on cardiac center to increase heart rate.
7. CORONARY CHEMOREFLEX:
(Bezold Jarisch Reflex) In experimental animals injection of some drugs e.g. serotonin, capsaicin and phenyl diguanides into coronary artery supplying left ventricle causes apnea followed by rapid breathing, hypotension and bradycardia – this is known as the coronary chemoreflex. Such a response is not observed with drug infusion into atria or right ventricle.
8. EXERCISE:
During anticipatory phase of exercise vagal inhibition causes increased heart rate. As exercise progresses sympathetic stimulation contributes to increased heart rate.
9. SLEEP:
During sleep HR is slowest.
10. PHYSICAL TRAINING:
increases vagal tone lowering the heart rate. Heart rate is lower in those who are physically fit.
11. TEMPERATURE:
Rate of SA node discharge increases with temperature increase.
12. HORMONES:
Thyroxine increases heart rate by increasing number of and affinity of β – adrenergic receptors in the heart thereby increasing its sensitivity to catecholamines. Hyperthyroidism cause tachycardia that persists during sleep while hypothyroidism results in bradycardia.
13. SINUS DISORDER: (SICK SINUS SYNDROME)
This occurs in the elderly and maybe due to SA node fibrosis or degeneration. It presents as bradycardia, sinus arrest with pauses, paroxysmal tachycardia and other forms of arrhythmias.
14. JAUNDICE AND RAISED INTRACRANIAL PRESSURE:
cause bradycardia.

CONCLUSION
The heart is a very delicate organ and the rate at which it supplies blood to the various organs is influenced heavily by a lot of factors. That is why it is advisable to engage in the following below to ensure the most optimum functionality of the heart:
Regular exercising: This ensures adequate tissue perfusion to the various organs and systems around the body.
Proper dieting: This involves eating foods such as lean meat, ovo-proteins and decrease in the consumption of trans fats and unsaturated fats which are known to cause coronary arterial diseases and atherosclerosis.
Rest and Sleep: This ensures adequate digestion of food substances and dissolution into the blood so that the heart can transport the digested food substances to the different parts of the body based on the needs of the body at that particular time.
I hope you learnt a thing or two about the heart rate and its regulation. Thank you for reading.

Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit