In my 10-year journey to manage my hypothyroid condition, I’ve learned that hypothyroidism diagnosis and treatment can be a little more complicated than what many mainstream doctors lead you to believe.
Here are 5 myths that I discovered the hard way.
- Myth: The TSH blood test is the quickest, most accurate, and conclusive way to determine if you have hypothyroidism.
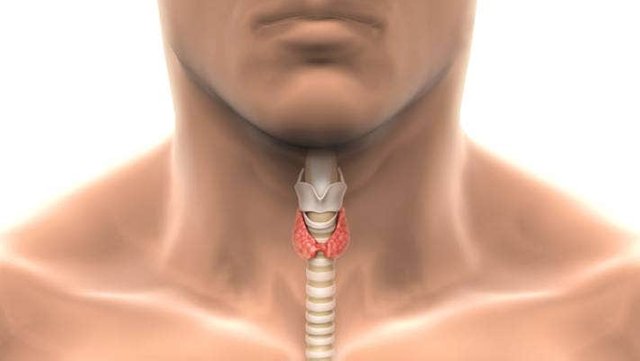
When I first expressed symptoms of hypothyroidism such as cold hands and feet, fatigue, weight gain, brittle nails, moodiness, menstrual problems, brain fog, and insomnia, my doctor ran a blood test called Thyroid Stimulating Hormone (TSH). According to mainstream medicine, TSH is the standard for the diagnosis and treatment of thyroid dysfunction.
My doctor found my numbers to be within ‘normal range’ and sent me away with anti-depressants, and sleeping pills, and told me to exercise more to relieve my symptoms. What I learned later was that the doctor had turned me away, undiagnosed, and left me suffering from debilitating symptoms which continued to worsen the longer they went unaddressed. Eventually, my TSH level fell outside the normal range and I was treated for hypothyroidism.
The reason that this can happen is that many doctors are using old lab ranges that underdiagnose hypothyroidism. The American Association of Clinical Endocrinologists (AACE) issued a press release in 2003 entitled “Over 13 Million Americans with Thyroid Disease Remain Undiagnosed”.
Until Nov 2002, doctors relied on a normal TSH level ranging from 0.5 to 5.0 to diagnose and treat patients with a thyroid disorder. Now AACE encourages doctors to consider treatment for patients who test outside the boundaries of a narrower margin, based on a target TSH level of 0.3 to 3.0.
AACE believes the new range will result in a proper diagnosis for millions of Americans who suffer from a mild thyroid disorder, that previously had gone undetected and untreated.
However, since the recommendation by AACE wasn’t widely published, today, 10 years later, many doctors are still using the old reference range resulting in continued under-diagnosis of the condition.
- Myth: Synthroid is the best hormone therapy to treat hypothyroidism.
Synthroid, and its generic version levothyroxine, are by far the most common drug therapies that doctors prescribe for hypothyroidism. Synthroid is a hormone replacement for T4. However, looking at thyroid function more closely, there are many other components to proper thyroid function than just T4.
When the pituitary gland in the brain releases TSH, TSH stimulates the thyroid gland to produce the thyroid hormones T4 and T3. The majority of thyroid hormones produced by the thyroid are T4.
However, T3 is the most active, useable form of thyroid hormone in the cells of the body. The conversion of T4 to T3 is critical. By testing TSH and T4 alone, doctors are assuming that our bodies are properly converting the T4 to active T3.
For many hypothyroid sufferers, myself included, the body does not convert T4 to T3 properly. In the care of doctors who only prescribed Synthroid or T4, my symptom did not improve; they just continued to worsen. It wasn’t until I finally switched doctors that my T3 levels were tested. I was then treated with natural desiccated thyroid resulting in significant improvement of my symptoms.
Even beyond TSH, T4, and T3, there are still other hormones that could be looked at. In Dr. Kharrazian’s book “Why Do I Still Have My Thyroid Symptoms”, he outlines 30 different scenarios in which various abnormal thyroid-related hormone levels can keep one feeling hypothyroid even when the TSH is normal. Other thyroid labs he recommends include TSH, Total T4, Free T4, Total T3, Free T3, T3 Uptake, and Reverse T3.
- Myth: A full thyroid panel is the quickest, most accurate, and conclusive way to diagnose and treat hypothyroidism.
After getting all of the previously mentioned levels within the normal range, I was still struggling. I would feel good for a few days, then crash for several more. What I didn’t know is that I also had the underlying autoimmune condition, Hashimoto’s, which was causing my thyroid levels to fluctuate as it attacked my thyroid. I learned that controlling my thyroid hormone levels with medication was not enough.
The National Endocrine and Metabolic Diseases Information Service admit that “Hashimoto’s is the leading cause of hypothyroidism”. The autoimmune attacks slowly begin to destroy the thyroid. With each attack over time, the need for higher doses of medication increases and fluctuates. If this underlying autoimmune response is not addressed, the attacks will eventually destroy the thyroid.
There are two lab tests used to detect the underlying Hashimoto’s called Thyroid Peroxidase Antibodies (TPOAb) and Thyroglobulin Antibodies (TgAb). However, these tests are not commonly done. Primarily because many mainstream doctors do not change their treatment once they make a diagnosis of Hashimoto’s since there are no effective drugs to stop the autoimmune response.
Fortunately, there are ways to calm the autoimmune response and there are knowledgeable doctors who can show you how, but you need to know how to find them!
- Myth: A full thyroid panel plus testing for the Hashimoto’s antibodies is the quickest, most accurate, and conclusive way to diagnose and treat hypothyroidism.
For some people, addressing the thyroid lab panels and underlying auto-immune response will finally give them relief and their symptoms will diminish. But, I wasn’t one of them. Yes, there is more. The problem is that the thyroid is only one component in a delicate balance of hormone systems that are part of our metabolism.
When one component is off, especially for a long duration of time or with no diagnosis followed by other missed diagnoses, this can throw off other parts of the body like our adrenals, liver, and more. Sometimes in order to really feel your best again, the doctor has to look at the person as a whole and determine ALL the pieces that need to come back in alignment.
Adrenal fatigue is common with thyroid sufferers and a little adrenal supplementation can make all the difference in how they feel. Iron and vitamin D deficiencies are common. Blood sugar levels might be off. Digestive issues are also common.
Other hormone imbalances can keep the hypothyroid patient from feeling their best. There are many other aspects that a doctor treating hypothyroidism/Hashimoto’s might have to look at to finally offer near-total relief of symptoms.
- Myth: When you have untreated hypothyroidism/Hashimoto’s, a low-calorie diet and regular exercise is the best way to lose weight.
Unfortunately, this perception is not only demeaning and harmful to the person who hears this, but it really isn’t true. What I found is that because of the underlying health issues, I was gaining weight. Resolving the underlying health issues automatically helps the weight fall off. For Hashimoto’s, changing my diet to avoid the foods that trigger the autoimmune response promoted my weight loss.
Some believe that the added weight is the body’s defense mechanism to protect itself from autoimmune attacks. No amount of calorie counting and exercise was helping me lose weight. Instead, I lost 7 lbs in 1 week when I started my diet to eliminate potential foods that could trigger my autoimmune attacks.
CAUTION: Now I need you to pay very close attention to this
Hypothyroidism is NOT the life sentence you think it is!
Most doctors think there is no cure for hypothyroidism. They’ll say you have to take drugs to control it for the rest of your life.

But this is not true anymore. Because it turns out there’s a root cause for hypothyroidism. And now there’s a cure for that root cause — a cure that’s been enjoyed by thousands of people around the world.
No more fatigue, no more depression, no more aching limbs, skin blemishes… and no more meds or visits to the doctor.
Read about this hypothyroidism solution here https://bit.ly/HypoNoMore — you’ll be so glad you did…