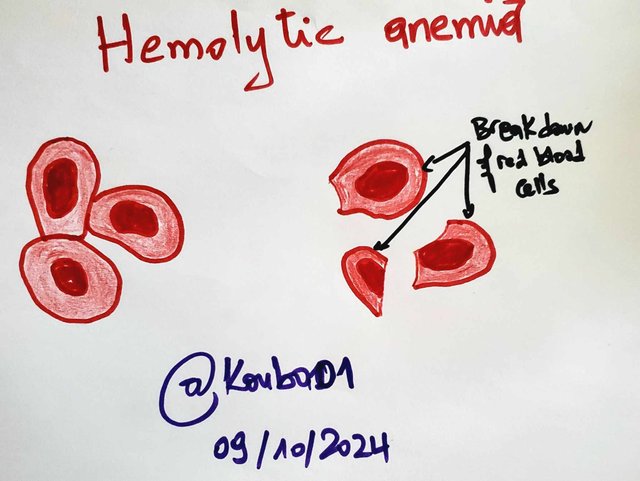
Define Hemolytic Anemias
I define hemolytic anemias as conditions where red blood cells are destroyed prematurely before completing their normal lifespan of about 120 days. This process of destruction is known as hemolysis. Hemolytic anemias can arise from internal issues within the red blood cells such as structural defects or from external factors like infections or medications. When red blood cells are destroyed faster than they are produced the bone marrow responds by producing immature red blood cells called reticulocytes. This is why hemolytic anemias are classified as regenerative as the body is constantly trying to replace the lost cells.
A high reticulocyte production index RPI over 3% is a marker of this regenerative process. Common symptoms include fatigue jaundice and shortness of breath. In severe cases an enlarged spleen may occur due to its role in clearing damaged cells from the bloodstream.
Define Sickle Cell Anemia
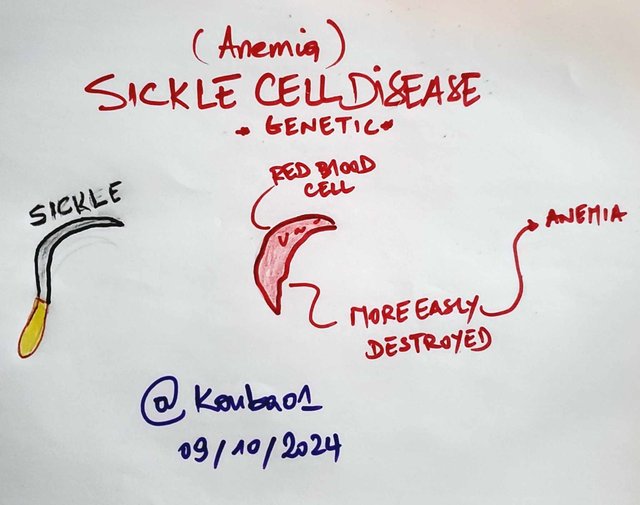
Sickle cell anemia is a genetic disorder caused by a mutation in the gene responsible for hemoglobin which results in the production of abnormal hemoglobin S. Red blood cells in sickle cell anemia adopt a crescent or sickle shape instead of the typical round form. This change makes them less flexible and more likely to block small blood vessels causing painful episodes called vaso-occlusive crises. These crises may last from a few hours to several days affecting areas like the bones abdomen and chest. Sickle cells also break down more easily leading to chronic anemia.
Sickle cell anemia is more common in people of African Mediterranean and Middle Eastern descent. Symptoms may include jaundice gallstones and an enlarged spleen. Over time the repeated destruction of these cells can damage the liver and other organs. Treatment often involves pain management hydration blood transfusions and medications like hydroxyurea to reduce the frequency of crises.
Intravascular Hemolysis vs Extravascular Hemolysis
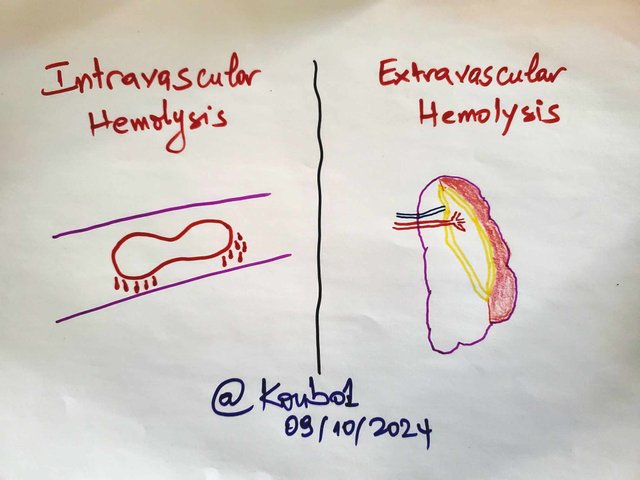
Intravascular hemolysis occurs when red blood cells are destroyed directly in the blood vessels. When the red blood cell membrane breaks hemoglobin is released into the bloodstream which can then be filtered by the kidneys and excreted in the urine causing hemoglobinuria or dark-colored urine. Hemoglobin can also bind to a protein called haptoglobin which transports it to the liver where it is broken down into bilirubin. If all haptoglobin binding sites are full hemoglobin may be converted into hemosiderin a toxic product that can accumulate in the kidneys.
Extravascular hemolysis occurs outside the blood vessels mainly in the spleen and liver where macrophages engulf and destroy old or damaged red blood cells. This process leads to the release of bilirubin which can cause jaundice. Extravascular hemolysis is often slower than intravascular hemolysis but can still result in anemia over time. This type of hemolysis is common in conditions like autoimmune diseases and hereditary spherocytosis where red blood cells are more fragile due to membrane defects.
Explain a case of Hemolytic Anemia
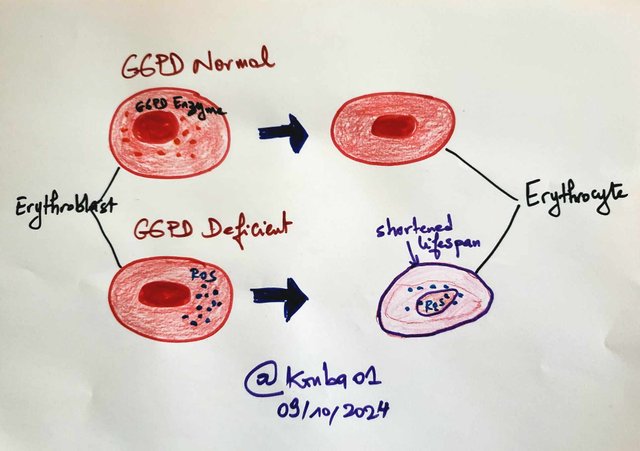
I remember a case involving a close friend of mine who was diagnosed with glucose-6-phosphate dehydrogenase deficiency, commonly known as G6PD deficiency. It’s a genetic condition that makes red blood cells much more sensitive to oxidative stress. My friend had been feeling extremely fatigued and noticed his urine had turned a dark color. He also had yellowing of the skin, which is a sign of jaundice. All of this happened shortly after he took some over-the-counter medication for a common cold. Naturally, he was concerned and went to see a doctor.
The doctor ordered blood tests, and they showed that his red blood cell count was quite low, while the number of immature red blood cells, called reticulocytes, was unusually high. This was a clear sign that his body was trying to compensate for the destruction of red blood cells, a process called hemolysis. The doctor quickly suspected G6PD deficiency, which can be triggered by certain medications, infections, or even foods like fava beans. In this case, the cold medicine he had taken set off the reaction that led to his red blood cells breaking down faster than they could be replaced.
To confirm the diagnosis, they performed a specific test to measure the G6PD enzyme, and the results confirmed that he did indeed have the deficiency. The treatment plan was straightforward but crucial. He stopped taking the medication immediately, and the doctors provided supportive care, including plenty of hydration to help his body recover. In more severe cases, a blood transfusion might be needed, but thankfully he didn’t need that. Over time, he started to feel better and recovered fully after avoiding triggers that could cause the same problem in the future.
This experience made us both realize how important it is to know about conditions like G6PD deficiency early on. If left untreated or undiagnosed, it could have led to more serious and potentially life-threatening complications. Now he’s very careful about the medications and foods he consumes to avoid similar episodes.
Thank you very much for reading, it's time to invite my friends @lil.albab, @miftahulrizky, @heriadi to participate in this contest.
Best Regards,
@kouba01

Upvoted. Thank You for sending some of your rewards to @null. It will make Steem stronger.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
THE QUEST TEAM has supported your post. We support quality posts, good comments anywhere, and any tags
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Saludos cordiales estimado amigo , como de costumbre, extraordinaria participación soportada con esquemas manuales muy certeros ; le felicito y le deseo merecidos éxitos en su gran participación.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit