Doctors and nurses at major Sydney hospital failed to properly wash hands when no one was watching, risking patients' lives: staff's hand-washing compliance rate dropped from 94% to 30% when human auditors stopped monitoring their behaviour and automated surveillance kicked in.
They are calling for an overhaul of the auditing system, which may still require human auditors because automated surveillance and reminder technology are expensive, and the re-education of hospital workers about the importance of hygiene.
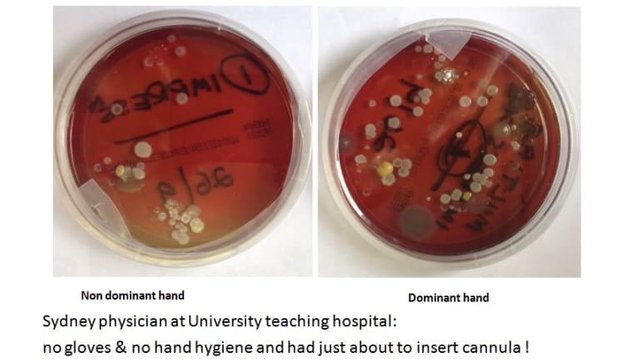
"Hand hygiene is the keystone to infection control that prevents healthcare workers from being colonised with a potentially life-threatening disease; that reduces hospital-acquired bloodstream infections that can kill up to 20 to 30 per cent of patients," lead author Mary-Louise McLaws said.
"Healthcare workers know how to respond when they’re being watched, but the rest of the time they go back to a dangerous level and I don’t blame them, no one's watching."
The results call into question the accuracy and effectiveness of Hand Hygiene Australia's (HHA) national program which largely relies on human auditors and has shown an increase in compliance from 64 per cent in 2010 to 84.4 per cent this year.
Between 2013 and 2017, cases of hospital-acquired 'golden staph', caused by Staphylococcus aureus bacteria, decreased by 12.5 per cent.
But Professor McLaws, an infection control expert, said the magnitude of the "Hawthorne effect" - the change in behaviour when people are watching - on human auditing produced "inflated" official compliance rates and all parties needed to go "back to basics".
The researchers used automated surveillance, which consisted of hand hygiene dispensers at sinks and bedsides that recorded hand hygiene by touch, to see how staff changed their behaviour. Compliance is based on the number of hand hygiene "moments" - opportunities when hand washing or cleaning ought to occur, whether before or after touching a patient.
The results call into question the accuracy and effectiveness of Hand Hygiene Australia's (HHA) national program which largely relies on human auditors and has shown an increase in compliance from 64 per cent in 2010 to 84.4 per cent this year.
“To date, no one has attempted to quantify potential errors in compliance rates,” Professor McLaws said.
"The healthcare workers need to have their behaviour flipped so that their hand hygiene is not centred on them and self-preservation but on the safety of others. We need a national behaviour change program."
HHA's Lindsay Grayson said the results from one hospital shouldn't be generalised to all 960 hospitals being audited across Australia.
“To date, no one has attempted to quantify potential errors in compliance rates,” Professor McLaws said.
"The healthcare workers need to have their behaviour flipped so that their hand hygiene is not centred on them and self-preservation but on the safety of others. We need a national behaviour change program."
HHA's Lindsay Grayson said the results from one hospital shouldn't be generalised to all 960 hospitals being audited across Australia.
"We're developing what we’re calling a patient safety model, which will broaden the education base of healthcare workers, so it will allow us to provide immediate observation and feedback throughout the day and night."
The study has been published in the American Journal of Infection Control.
Hi! I am a robot. I just upvoted you! I found similar content that readers might be interested in:
https://www.smh.com.au/healthcare/hospital-doctors-neglect-washing-hands-hygiene-20180706-p4zpvv.html
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit