Even after the pandemic was declared over almost a year ago serum antibody titers, which is not a measure of immunity, have continued to consume the media’s attention span with little regard to substantial risk factors for infection outcome other than age and immunocompromising conditions such as obesity, diabetes and various pulmonary and cardiovascular disorders. Sparsely mentioned is the critical role of vitamin D, specifically vitamin D3, and its metabolites in strengthening the adaptive immune system mainly through the vitamin D receptors of several types of immune cells. I briefly covered this in Why Vitamin D Is Necessary for Adaptive Immune Response. What I haven’t covered is the plethora of evidence that higher vitamin D concentrations in the blood, especially compared to people below the sufficiency threshold 50 nanomoles/liter, reduces the risk of infection, severe disease requiring hospitalization and/or ICU admission and mortality.
A large retrospective cohort study of VA patients, published in Nature, who supplemented vitamin D3 and Vitamin D2 prior to SARS-COV-2 infection matched with an equal number of untreated control pairs (n = 465,428) found that patients that supplemented with vitamin D2 and D3 prior to and during the pandemic, but not after infection, had a 20 and 28% lower relative risk of SARS-COV-2 infection compared to matched untreated controls and a 25% and 33% lower relative risk of COVID19 mortality within 30 days of infection. Both results were statistically significant at the 0.001 alpha level but only for vitamin D3 supplementation. The associated relative risk reduction of infection was similar between male and female VA patients but greater for black patients (29%) than white patients (18%) independent of vitamin D blood levels. The relative risk reduction of SARS-COV-2 infection was inversely proportional to Vitamin D blood levels with the highest risk reduction between 0-19 nanograms/milliliter followed by 20-39 nanograms/milliliter and tapering off above 40 nanograms/milliliter. Based on these findings, the authors estimate that D3 supplementation could have resulted in 4 million fewer COVID19 cases and 116,000 fewer COVID19 deaths in 2020.
An RCT of hospitalized COVID19 patients at Reina Sofia University Hospital in Spain (n = 76) found that half of the patients treated with the standard of care at the time (400 mg HCQ 2x daily and 200 mg 2x daily for 4 days plus 500 mg AZ for 5 days) required ICU admission compared to only 4% of patients treated with calcifediol. None of the patients treated with calcifediol died and all were discharged without compilations while 2 patients in the standard of care arm died. Another RCT of COVID19 patients with moderate to severe disease randomized to receive 600,000 international units cholecalciferol or placebo (n = 90) found that the former had a better sequential organ failure assessment score on day 7 of treatment and a lower 28-day mortality rate (24%) compared to patients in the placebo arm (44%). The mortality rate difference was statistically significant at the 0.05 alpha level while the sequential organ failure assessment score difference was statistically significant at the 0.01 alpha level.
A recent systematic review RCTs conducted on Vitamin D supplementation (PRISMA Study) (n = 7), also found that Vitamin D supplementation was inversely associated with infection risk with 5 RCTs conducted among healthcare workers finding an overall 80% relative risk reduction while the two studies conducted among patients found no effect on infection rate, although as the authors note this may be due to low prevalence of vitamin D deficiency in the study population as at least one RCT had no control cohort and only compared different regimens.
A prospective clinical cohort study conducted among patients in 8 COVID19 units within a Barcelona hospital (n = 838) found that patients treated with calcifediol (2x266 microgram capsules at baseline with follow up single capsule doses at days 3, 7, 15 and 30) were less likely to be admitted to ICU (4.5%) compared to patients treated with only the standard of care (21%). While ICU patients had significantly lower baseline calcifediol blood concentrations (median 10 ng/mL) compared to patients who stayed in the regular COVID19 ward (median 13 ng/mL) patients treated with Calcifediol had an 87% reduction in relative risk of ICU admission when adjusting for differences in age, sex, comorbidities and baseline calcifediol blood concentrations. Patients with adequate calcifediol blood concentrations of at least 20 ng/mL or more had a 70% decreased risk of ICU admission compared to patients with Calcifediol blood concentrations below that threshold. Patients treated with the oral calcifediol were also far less likely to die with COVID19 (4.7%) compared to patients treated with the standard of care (15.9%) which translates into a 70% reduced risk of COVID19 mortality adjusting for age, sex, comorbidities and baseline Calcifediol blood concentrations.
A retrospective analysis of antigen test results between March and June 2020 matched with the most recent vitamin D3 blood level test results from the prior 12 months (n = 191,779) found a strong inverse correlation between SARS-COV-2 positivity and circulating calcitriol (r2 = 0.96). Antigen positivity was 35% lower for patients with adequate calcitriol levels, defined as at least 30 ng/mL, compared to vitamin D deficient patients below the 20 ng/mL threshold while the positivity rate was 27% lower for patients with levels of at least 55 ng/mL compared to patients with adequate levels of 30-34 ng/mL. These differences were statistically significant at the 0.001 alpha level. The decrease in antigen positivity rate plateaued as circulating calcitriol levels approached 55 ng/mL
A retrospective study that used seasonally adjusted (see Methods section for details) pre-infection calcifediol blood concentrations from the medical records of COVID19 patients treated at Galilee Medical Center (Israel) between April 2020 and February 2021 14-730 days prior to diagnosis (n = 253) found that patients with sufficient vitamin D levels above the 20 ng/mL threshold had a much lower COVID19 mortality rate (2.3%) compared to vitamin D deficient patients below that threshold (25.6%). Patients with vitamin D deficiency measured below the aforementioned threshold were also 14x more likely to suffer severe or critical disease than patients with vitamin D levels at or above the sufficient threshold. Disease severity was also inversely correlated with vitamin D levels between the sufficient threshold of 20 ng/mL and the adequate threshold of 40 ng/mL with patients closer to the adequate threshold more likely to experience mild disease compared to patients closer to the former threshold.
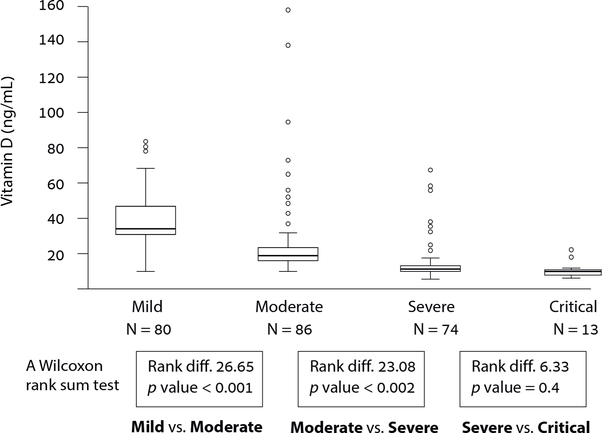
Only 8.8% of patients who experienced mild symptoms had less than 20 ng/mL vitamin D while such patients were 58.1% of patients who experienced moderate disease and 86.5% of patients who experienced severe disease.
A meta analysis of prospective and retrospective studies of the association between vitamin D concentrations and SARS infections, ICU admissions, and mortality (n = 54), published Frontiers, found that Vitamin D deficiency is associated with SARS-COV-2 infection at the time of testing in 16 studies and before testing in 7 studies. Severe vitamin D deficiency, defined as concentrations below 25 nanomoles/liter, were found to be associated with COVID related hospitalization when measured before hospitalization in 2 studies and when measured at the same time as a SARS-COV-2 test in 3 studies. Severe vitamin D deficiency was also associated with ICU admission when measured at the time of hospitalization in 10 studies and before hospitalization in 1 study. Even vitamin D3 concentrations below the thresholds of 50 nanomoles/Liter and 75 nanomoles/liter were associated with ICU admission when measured at the time of hospitalization in 14 studies and 10 studies respectively. One study found that Vitamin D insufficiency was associated with acute respiratory distress syndrome (ARDS) and sepsis in senior patients (65 or older) when measured before hospitalization. Severe vitamin D deficiency was associated with higher COVID19 mortality when measured at the time of hospitalization in 19 studies.
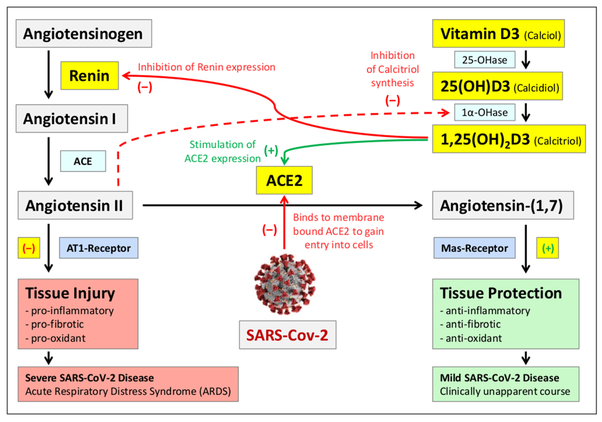
Mendel and colleagues note that vitamin D3 can reduce the risk of SARS induced acute respiratory distress syndrome through its role in the renin-angiotensin system by inhibiting renin expression which in turn inhibits angiotensin 2 synthesis and stimulates ACE2 expression that is otherwise diminished by the SARS-2 virus which increases angiotensin 2 levels and therefore the risk of acute respiratory distress syndrome. The list 5 other immune boosting mechanisms including reducing cytokine release through differentiation of regulatory T-cells and inducing the production of antimicrobial peptides in macrophages and epithelial cells of the lungs making target cells less viable hosts for replication.
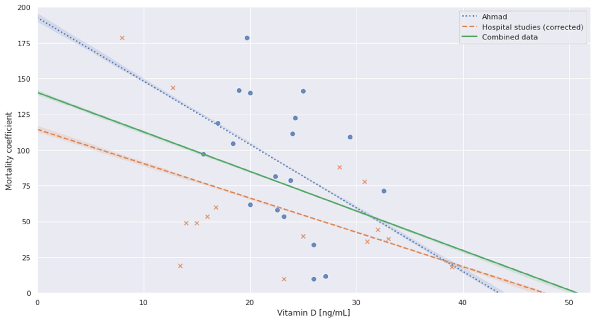
In their subsequent meta-analysis (n = 8) they found that COVID19 mortality rate approached zero at 40 ng/mL calcitriol levels (the adequate threshold) and was virtually zero at 50 ng/mL or approximately 125 nanomoles/liter.
As Quesada-Gomez and colleagues note in their article published in The Journal of Steroid Biochemistry and Molecular Biology, the body uses vitamin D3 (calcifediol) available in the blood to synthesize calcitriol has a role in controlling inflammatory responses to pathogens in the lungs through the vitamin D receptors on immune cells such as lymphocytes, monocytes, macrophages and alveolar type II cells diminishes cytokine storms, modulates neutrophils, maintains pulmonary/epithelial barriers, stimulates epithelial repair and decreases the risk of hypercoagulation and pulmonary blood clots. A rodent study, published in Nutrients, found that high doses of Vitamin D in its active D3 form reduced lung inflammation in mice infected with SARS-COV-2. Vitamin D deficient mice had more severe lung inflammation, respiratory symptoms, and longer time to recovery compared to Vitamin D sufficient mice and vitamin D deficient mice dosed 2.5 micrograms daily for 8 weeks prior to infection. They also found that vitamin D deficiency alone results in lung inflammation without infection.
This is not the totality of evidence for Vitamin D, specifically in its active form, as a COVID19 prophylaxis but only a cross section of the literature on its role as a predictor of infection and disease severity and the mechanisms by which it can reduce it. Read more:
Vitamin D Supplementation and COVID19 Outcomes: Mounting Evidence and Fewer Doubts