 The digital rectal examination (DRE; Latin: palpatio per anum, PPA) is a relatively simple procedure. The patient undresses, then is placed in a position where the anus is accessible (lying on the side, squatting on the examination table, bent over the examination table, or lying down with feet in stirrups). During this procedure, areas which can be palpated are: the bulb of the penis, the urogenital diaphragm, the anorectal ring, and other nearby anatomical landmarks. However, structures like the ureter (the two tubes that run from each kidney to the urinary bladder), and the urethra (which, in a male, is divided into three parts, and is inside the penis) cannot be palpated.
The digital rectal examination (DRE; Latin: palpatio per anum, PPA) is a relatively simple procedure. The patient undresses, then is placed in a position where the anus is accessible (lying on the side, squatting on the examination table, bent over the examination table, or lying down with feet in stirrups). During this procedure, areas which can be palpated are: the bulb of the penis, the urogenital diaphragm, the anorectal ring, and other nearby anatomical landmarks. However, structures like the ureter (the two tubes that run from each kidney to the urinary bladder), and the urethra (which, in a male, is divided into three parts, and is inside the penis) cannot be palpated.
If the patient is lying on his side, the physician will usually have him bring one or both legs up to his chest. If the patient bends over the examination table or the back of a chair, the physician will have him place his elbows on the table and squat down slightly, generally a man having his prostate examined can expect it to be examined in the bending position as it is easier to conduct the examination with a man standing. If the patient uses the supine position, the physician will ask the patient to slide down to the end of the examination table until his buttocks are positioned just beyond the end. The patient then places his feet in the stirrups.
The physician spreads the buttocks apart and will usually examine the external area (anus and perineum) for any abnormalities such as hemorrhoids, lumps, or rashes. Then, as the patient relaxes, the physician slips a lubricated finger into the rectum through the anus and palpates the insides for a short time (from about 5 to 60 seconds).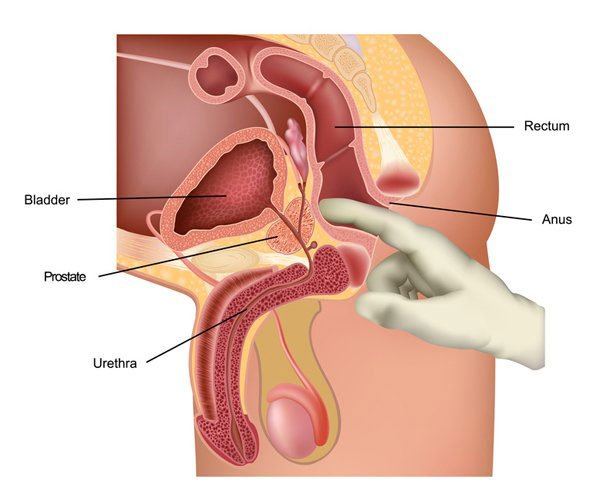
This examination may be used:
for the diagnosis of rectal tumors and other forms of cancer;
for the diagnosis of prostatic disorders, notably tumors and benign prostatic hyperplasia,[1][2] but the DRE frequently misses more early-stage tumors than prostate-specific antigen (PSA) among African American and Caucasian men. If PSA is positive (frequently false positive), then DRE can be done to reduce the false positive;[3]
for the diagnosis of appendicitis or other examples of an acute abdomen (i.e. acute abdominal symptoms indicating a serious underlying disease);
for the estimation of the tonicity of the anal sphincter, which may be useful in case of fecal incontinence or neurologic diseases, including traumatic spinal cord injuries;
in females, for gynecological palpations of internal organs;
for examination of the hardness and color of the feces (i.e. in cases of constipation, and fecal impaction);
prior to a colonoscopy or proctoscopy;
to evaluate hemorrhoids;
in newborns to exclude imperforate anus.
through the insertion of medical devices including thermometers or specialized balloons; to identify digestion problems, parasites, organ damage, anal bruising, and foreign objects in the rectal cavity.
The DRE is frequently combined with an FOBT (fecal occult blood test), which may be useful for diagnosing the etiology of an anemia and/or confirming a gastrointestinal bleed.
The DRE is inadequate as a screening tool for colorectal cancer because it examines less than 10% of the colorectal mucosa; sigmoidoscopy is preferred. However, it is an important part of a general examination, as many tumors or other diseases are made manifest in the distal part of the rectum.
Sometimes proctoscopy may also be part of a rectal examination.
Hi! I am a robot. I just upvoted you! I found similar content that readers might be interested in:
https://en.wikipedia.org/wiki/Rectal_examination
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit