Hey, everyone..
I will now share a topic that often does not occur as often as other clinical entities, and that its medical diagnosis and management is a challenge.
As we know, malaria is the parasitic disease that needs a vector in this case the bite of the mosquito of the genus Anopheles carrying Plasmodium with its infectious form to be able to replicate in man and cause disease.
Currently, more than 150 thousand species of Plasmodium have been described, but only 4 are capable of generating disease in man, and these are: Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae and Plasmodium ovale.

Public domain by health.mil
In this last decade, cases of malaria caused by Plasmodium knowlesi have been reported, being a species previously exclusive to the macaque monkey, but in areas that are the habitat of this animal and that have been populated by man, this parasite has taken on the capacity to take man as a host and generate the disease.
Although, this pathological entity by itself, has generated a high rate of incidence and mortality is the result of a failure in the treatment, by mixed infections, the immunological state of the host in this case the man, and by failures in the epidemiological system in the prevention of this disease.
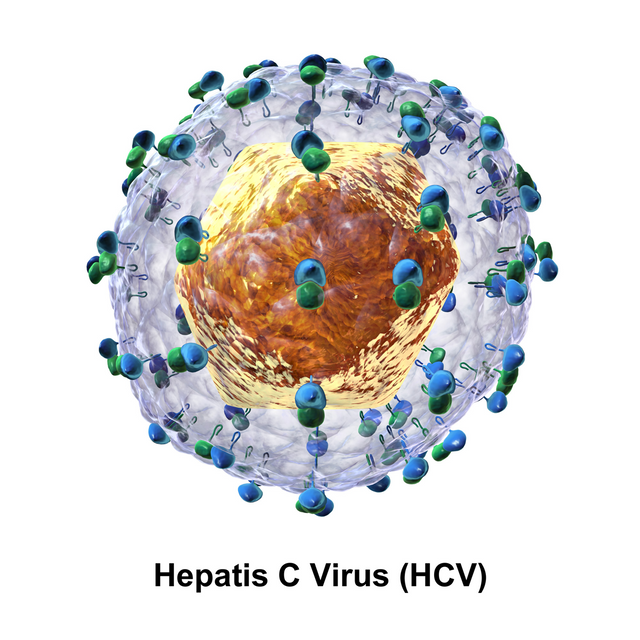
Now, associated to the Hepatitis "C" Virus (HCV), which is originated by a totally different etiological agent, being this an RNA virus of the Hepacivirus genus from the Flaviviridae family. Its mechanism of transmission is more complex in relation to other hepatitis viruses such as HAV and HBV, it reaches the hepatocyte where it replicates through blood transfusions, intravenous drugs, reuse of non-sterile syringes, sexual relations, among others.
The present clinical case, was brought with the purpose of making known that it is possible and viable the coexistence of these pathological entities, despite being totally different etiological agents has in common its reproduction cycle for life as it is the hepatocyte.
Public domain CC BY-SA 4.0
Clinical case
A 30-year-old male patient, with no significant pathological history, is admitted to the emergency unit. He started the current disease approximately 2 months ago, characterized by unquantified heat waves without a predominant time schedule, preceded by chills, which partially subsided with common antipyretics, accompanied by frontal headache of strong intensity, of oppressive character, retro ocular pain and photophobia, likewise it is associated finally with liquid evacuations in number of 4 per day, without mucus, without blood, in view of symptomatology it is taken to the emergency where it is admitted, for 18 days during its intrahospital evolution multiple paraclinical studies are requested. He was treated for 3 days with metronidazole and ceftriaxone for 8 days, plus an animal-based scheme for 3 days. He is then discharged with clinical improvement. After one week, the feverish picture reappears with 39º C without prevalence of time, preceded by shivers, which partially disappears with common antipyretics, concomitant asthenia, hyporexia, and he is admitted again.
Some important patient history:
Habits:
Functional test:
Physical Entrance Examination:
Patient Stable Clinical Conditions, afebrile to touch, hydrated, eupneic, skin and mucous membrane colored, tolerating oral, and ambient oxygen. Normocephalic skull, isocoric pupils reactive to light. Mobile neck without adenopathies.
Symmetrical thorax, normo-expanding, RsCsRs without presence of murmur, audible breathing sounds in both hemi thorax, no added auscultation.
Painful depressible soft abdomen on superficial and deep palpation in right hypochondrium, RsHsAS present with mild hepatosplenomegaly.
Symmetrical extremities without edema. Neurological: conscious oriented in time, space and person.

Public domain Wikipedia
Relevant paraclinic of the 1st hospitalization:
Serologies
However, he presents again 8 days after his discharge, fever, headache, myalgia and arthralgia, so he is reevaluated and admitted.
Paraclinic of 2nd hospitalization.
Serologies
Thick drop in 7 occasions, evidencing in the 2 positive thick drop control for P. falciparum. It was decided to start treatment again in animals.
Ultrasounds in 2 opportunities
1st Report mild hepato-plenomegaly.
2nd elaborated by the Gastroenterology service: Hepatic Steatosis grade I Splenomegaly.
Intrahospital evolution
Patient who during his intrahospital evolution, remains feverish, quantified in 38.The first two weeks, at the time of admission, third generation cephalosporin was indicated, but without criteria it was omitted on the fourth day. A paraclinic was performed in search of an infectious focus or the cause of the feverish picture, among which a blood biometry was requested, which was evaluated by the hematology service where red blood cells were found to be parasitized.
Physical examination showed hepato-plenomegaly, and with a negative first large drop, a GRL evaluation was requested for ultrasound, where grade I hepatic steatosis and splenomegaly were reported.
The patient, after completing the animalarium scheme, showed a feverish peak, with evident focus of skin and soft tissues (phlebitis at the site of venipuncture), which resolved with topicals. The patient is discharged from the hospital with satisfactory outpatient gastroenterology and internal medicine controls.
Clinical case discussion
It is interesting to note that this patient was initially diagnosed with Dengue Fever on his first hospitalization, with signs of alarm due to both symptoms and paraclinical admission, with a torpid intrahospital evolution associated with enteral disease due to liquid evacuation for more than 10 days, as well as nosocomial respiratory infection, multiple pathological entities, which were treated together with a thick drop positive for P. falciparum.
It is very probable that in this first opportunity that the patient receives animal treatment, he attended with enteral picture given by liquid evacuations of more than 5 per day accompanied by nausea and vomits, therefore, the absorption and excretion of drug was not the correct one being evidenced only a partial improvement with a minimum load of parasites nondetectable in the control drop.
Physiopathology
As mentioned above, both the malaria parasite and the hepatitis C virus require the hepatocyte to fulfill part of their life cycle.
)
Life Cycle of the Malaria Parasite. Public domain wikipedia
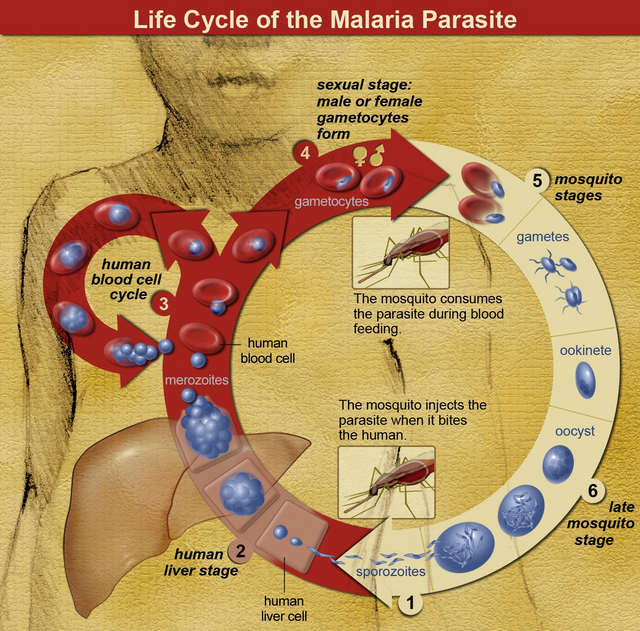
In relation to Malaria, this etiological agent needs two hosts to complete its complete cycle, in this case Anopheles (mosquito) and Man who is the accidental host.
Once the Plasmodium completes its cycle in the host, its infectious form lodges in the salivary glands of the mosquito which is inoculated during the bite, this enters the bloodstream in the form of sporozoites and goes to the hepatocyte, and according to the infectious species, it can continue its replication and transform into merozoites or remain in latent form as hypnozoites, only in the case of P. Vivax and Ovale. Once it leaves the hepatocyte it goes to the erythrocyte and becomes a trophozoite.
In relation to HCV it also cycles in the hepatocyte, and that both Plasmodium and this virus bind to the hepatocyte through membrane receptors sharing one in common as is CD-81, generating greater competition and severity of the disease by excessive increase with the need to replicate and take more easily the union to the hepatocyte, causing competition and severity of the disease.
Diagnosis and treatment
The diagnosis is simple for both diseases, in the case of malaria it is done by means of a direct smear examination under the microscope or also called coarse drop, it is the standard gold.
The hepatitis C virus is serological (antigens of HCV) simple and rapid and if positive we must request the viral load (RNA) of the same to determine whether to initiate treatment or not. It is advisable to complement the paraclinic with ultrasound, tomography if necessary and even liver biopsy, where the diagnosis is uncertain.
Regarding treatment, for malaria it will depend on the species observed in the thick drop and its presentation if it is uncomplicated or complicated malaria.
Finally, HCV can remain asymptomatic for years and even decades to generate disease, with more than 80% of cases originating from liver cirrhosis and hepatocarcinoma. Those cases of acute presentations or with high viral load should begin treatment.
Conclusion
Both malaria and HCV are diseases that represent a global health problem, and their coexistence generates atypical and cumbersome presentations of these medical entities.
We must bear in mind that the liver is the target organ, both for the plasmodium parasite and for the hepatitis C virus, which is why its function must be constantly monitored, by means of laboratory tests, (TGO, TGP, Bilirubins, GGT, coagulation times, glycaemia, proteins, among others) and the patient's clinic that make us think of liver failure.
In view of all the above, the need arises to diagnose on time, treat correctly, avoid complications that may be generated and preserve the life of the patient.
Sources:

steemSTEM is a project of the chain of blocks that supports the scientific content in different areas of science. If you want to know more about this wonderful project you can join the server in discord
This article will be published at https://www.steemstem.io/
link
If you have any questions about any topic of medicine or present any disease you can comment the publication or write me in discord and I will attend you.
Dr. Ana EstradaI hope you enjoyed my content.
Hello,
I found this very interesting, from the perspective of a medical consumer. I know your blogs are more or less advisories for practitioners, but this one also has valuable information for potential patients.
Medical students, I've been told, are supposed to look for 'horses', not 'zebras'--the usual, not the unusual. Unfortunately, often precious time is lost because a doctor doesn't look for the unlikely. So, if a patient is aware, then perhaps if a zebra is in closet the patient might alert the doctor to the possibility.
My principle, in healthcare is that patients are partners with doctors. Thanks for helping to facilitate that partnership.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Hi, thank you. I'm really glad you're enjoying my content. In a way it's quite an unusual pathology that's why I decided to share it.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
I actually have never seen P. knowlesi under the scope before. That’s something I didn’t know that happened.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
In some ways it is a very rare disease, but it is real and its extent has been demonstrated, both malaria and hepatitis can coexist @enforcer48
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
malaria and hepatitis this is an impressive and at the same time terrifying that can appear within the same pathology.
Thanks por sharing @anaestrada12
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Indeed, dear Carlos, thank you for reading my post
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Thanks for having used the steemstem.io app and included @steemstem in the list of beneficiaries of this post. This granted you a stronger support from SteemSTEM.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Thank you very much @steemstem
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit