Hemophilia is a blood condition. Actually, it is the most well - known blood disease in the world, simply because it affects a great number of people out there. One of the things that make hemophilia much more dangerous than your average blood problem is the fact that it is a genetic disease. That means that there is something essentially wrong with your body, starting at a chromosome level and working its way up. Also, hemophilia is an inherited disease, mostly, and a very hard to control one.
Hemophilia - An introduction
What really strikes your mind when you hear the word Hemophilia? Well, the origin of this word is from Greece. This is the combination of two words "Hemo" and "Philia" meaning "Blood" and "Love".In ancient times people thought people with this condition loved to bleed or we can say it was hard for the people to stop bleeding. All this happens because a process called "Hemostasis" is faulty. Before we go into the topic "Hemophilia" we must know what hemostasis is.
Hemostasis
Hemostasis is a very important and natural process whose main function is to stop the bleeding when an injury to blood vessels occurs. There are 3 mains processes for this to occur.
- Vasoconstriction
- Platelet adhesion
- Finally coagulation
Primary Hemostasis :
This process includes Vasoconstriction and Platelet adhesion. Whenever there is an injury to the blood vessel, vasoconstriction happens in a very short time, this limits the bleeding. Which proceeds to platelet adhesions to the injured site. This triggers more platelet aggression which later proceeds to Secondary hemostasis.
Secondary Hemostasis :
This is the process that really stops bleeding. There are many clotting factors floating around in the blood. Most of these factors are liver synthesized protein. But how is coagulation cascade triggered? Well, when one of the proteins is proteolytically broken down, break down another protein and the cascade starts. There are two ways these cascade stars.
- Extrinsic Pathway
- Intrinsic Pathway
Extrinsic Pathway
I will explain this pathway in points so that it will be easy to understand.
- when there is an injury to blood vessels, tissue is exposed thus exposing tissue factor or factor III
- Tissue factor or factor III activates factor VII also known as a stable factor to Factor VIIa.
- Active Factor VIIa combines with Tissue factor to activate Factor X to Factor Xa
- This Factor Xa combines with co-factor Va which activates Factor II also known as Prothrombin to Factor IIa (Thrombin).
- Factor IIa converts Factor I also known as Fibrinogen to Factor Ia (Fibrin).
- Thrombin or Factor IIa also converts Factor XIII to Factor XIIIa which with fibrin forms a stable clot.
Note: Fibrinogen is soluble and Fibrin in insoluble which leads to clotting.
Intrinsic Pathway
I know it's hard but stay with me.
- This starts from the platelets attached to the injured site.
- This activates Factor XII to XIIa.
- Which leads to activation of Factor XI to XIa
- Which in turn activates Factor IX to IXa
- This activated factor IXa combines with Factor VIIIa to activate Factor X to Factor Xa.
- From this point, this continues the same path as the Extrinsic pathway. (From Point number 4 of Extrinsic Pathway)
Fig : Coagulation cascade showing both Intrinsic and Extrinsic pathway (Source)
Now, How does Hemophilia occur?
Hemophilia is a genetic disorder so really the defect is at the chromosome level which can cause the deficiency of any clotting factors mentioned above. But there is an exception if there is a deficiency of factor XII, its mostly asymptomatic. The most common Deficiencies are Factor VIII, Factor IX, von-Willebrand factor, vitamin k deficiency which leads to deficiency of liver formed clotting factors. Let's describe these factor deficiencies now.
Hemophilia A ( Deficiency of Factor VIII)
There are many types of hemophilia out there, but the most common and notorious one is hemophilia A. Known also as classic hemophilia (or factor VIII deficiency), hemophilia A is a mostly inherited condition. When a patient suffers from classic hemophilia, his or her body does not have a protein (factor VIII) which is needed for the process of forming blood clots when a persons' blood is too thin. This lack of factor VIII leads to certain problems, like the very real possibility of bleeding out due to the fact that your bleeders will not close. However, even if hemophilia A is a condition passed down through generations commonly, that does not mean that it cannot be developed spontaneously, at the moment of conception, due to an unexpected gene mutation. About 30% of classic hemophilia patients have no relatives with the same condition.
Symptoms
Most classic hemophilia patients are diagnosed from birth when they manifest certain undeniable symptoms: bleeding into the surrounding tissue of the main arteries and veins and excessive bleeding after the umbilical cord has been cut or after a male child is circumcised. Unfortunately, all of these symptoms only get worse with age: thus, the bleeding episodes start to become much more frequent, the bleeding inside the joints or muscles gets very painful and uncomfortable and the danger of the patient dying from a routine procedure becomes obvious.
Hemophilia B (Christmas Disease)
Hemophilia B, also known as factor IX deficiency or Christmas disease, is the second most common type of hemophilia in the world. The reason behind its rather unusual nomenclature, "Christmas disease", is that the first patient with hemophilia B was diagnosed around Christmas, in 1952.
In the case of Christmas disease, the body lacks not factor VIII protein, like for hemophilia A, but factor IX protein. Unfortunately, this type of hemophilia cannot be called milder, since the missing protein has the same effect on the body as factor VIII. Without it, the body of the sufferer cannot form blood clots, thus cannot stop the bleeding from turning disastrous in certain conditions.
Symptoms
Hemophilia B symptoms include pain in your joints, stiffness, the darkening of the area around your veins and arteries due to blood leaking into the tissues and unusual amount of blood loss after minor cuts and bruises. But it can be very difficult to distinguish it from Hemophilia A, Hemophilia C
Hemophilia C
Hemophilia C, also known as factor XI deficiency, is the rarest form of hemophilia because it is the only that is race-oriented. Factor XI deficiency is something that the medical world calls a "double - trouble": this factor is a protein produced in the liver. It not only controls, in itself, a part of the coagulation process, but it is also a precursor of another hugely important protein, the well-known factor IX (the lack of this protein produces hemophilia B). So, people who lack factor XI suffer from a very serious form of hemophilia, usually hard to control and even harder to treat accordingly.
Symptoms
Unlike classic hemophilia and hemophilia B, this version of the feared blood disorder has no standard symptoms. Unfortunately, the signs that precede the bleeding episodes are not identical, not even for family members that suffer from this type of hemophilia. This is not good news for anyone involved, because it takes a series of very serious bleeding episodes for the patient to be able to read his or her own body and prevent the attack and the medical doctors never know what to be on the lookout for when they have an unconscious patient with hemophilia C. There is no known cause of why the symptoms vary so much from patient to patient. The only way of predicting that that person might be affected is to check their factor XI levels and see if they are below 15%.
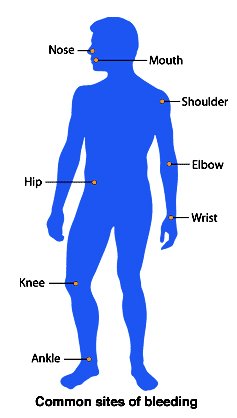
Fig: Most common Bleeding Sites (Source)
Treatment for Hemophilia
For now, there is no actual cure or treatment for this disease. Nowadays, the hemophilia cure is a lab rat away for some. For others, the hemophilia cure might take a while to reach them, but it is coming, that is a certainty.
Today, the only treatment for hemophilic patients is to replace the missing clotting factors. These clotting factors are injected into the person's vein which helps in clotting of blood.
Medications
Yes, there are some medications available that give periodic relief from this disease. Some of them are
Clotting Factors
- Plasma-derived clotting factors
- Recombinant clotting factors
Plasma-derived clotting factors:
Plasma is just a part of our blood or you can say the liquid part. This liquid part contains many proteins such as clotting factors and antibodies. SO, as the name suggests clotting factors are derived from the plasma. Many people contribute to the collection of plasma.
Recombinant clotting factors
This is a newer approach for making clotting factors. In this approach DNA recombinant technology is used to make clotting factors.
You stayed until the end. Thank you so much for reading guys hope you enjoyed it. Also Dont forget to visit my site .
References :
[1] https://www.cdc.gov/ncbddd/hemophilia/facts.html
[2] https://ghr.nlm.nih.gov/condition/hemophilia ncell mero plan
Very Informative.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Congratulations @idoctor! You have completed the following achievement on the Steem blockchain and have been rewarded with new badge(s) :
You can view your badges on your Steem Board and compare to others on the Steem Ranking
If you no longer want to receive notifications, reply to this comment with the word
STOPTo support your work, I also upvoted your post!
Do not miss the last post from @steemitboard:
Vote for @Steemitboard as a witness to get one more award and increased upvotes!
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
This post has been voted on by the SteemSTEM curation team and voting trail. It is elligible for support from @curie and @minnowbooster.
If you appreciate the work we are doing, then consider supporting our witness @stem.witness. Additional witness support to the curie witness would be appreciated as well.
For additional information please join us on the SteemSTEM discord and to get to know the rest of the community!
Please consider using the steemstem.io app and/or including @steemstem in the list of beneficiaries of this post. This could yield a stronger support from SteemSTEM.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
A very complete content. Very well developed explanation of this pathology
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
You explained the physiology and the different variants extensively but were quite short on the medications (what affected people would be interested most in I guess). Most significantly there is a new, promising mode of action (instead factor replacement) led by Emicizumab which is given subcutanously instead of i.v. - a milestone in patient convenience.
https://en.wikipedia.org/wiki/Emicizumab
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Emicizumab
Emicizumab (trade name Hemlibra) is a humanized bispecific antibody for the treatment of haemophilia A, developed by Chugai (a subsidiary of Roche). A Phase I clinical trial found that it was well tolerated by healthy subjects.In November 2017, it was approved by the US FDA for treatment of haemophilia A in those who had developed resistance to other treatments. It was subsequently approved by the US FDA in April 2018 under the breakthrough therapy designation for treatment of haemophila A in those who have not developed resistance to other treatments.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
It’s nice to see a medical content on steemit !
Nice to met you !
(I’m a medical student to)
Posted using Partiko iOS
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit