Hi Steemians!
Continuing the previous topic on what to do in case of injuries, burns and poisoning, today will be explained on how to provide first aid in the emergencies that occur most, in this case of fainting, fevers, asphyxia, stings and bites.
Stings and bites.
All animals are conditioned to different stimuli in search of food, reproduction, survival and not to be preyed upon by others, creating strategies, such as mimicry, with nature around them. It is there, due to our ignorance of their habitat, where we accidentally get into a tree or when we put our hands under a stone.
The bites and bites are considered as injuries that initially affect the soft tissue but that according to the evolution and the organic response of each individual, can affect all systems, even causing death if the attention is not fast and adequate, especially in people who suffer severe allergic reactions.
Stings.
The stings are small puncture wounds produced mainly by insects, arthropods and marine animals, through which they inject toxic substances that act locally and systematically throughout the body, according to the kind of causative agent, the amount of toxic and the organic response
Stings of bees, wasps and ants. The bites of these insects are the most frequent. Occasionally they can cause death, almost always due to the acute allergic reaction produced by the poison they inoculate. The wasp and the ant can use its sting repeatedly, while the bee, especially the honey producer, leaves its sting and the poisonous sac adhered to the skin of the victim.

Source
- Signals
Not all people react in the same way to these bites. The demonstrations can be local or general.
a) Locals. They occur more frequently and can be:
• Pain
• Inflammation in the form of a white blister, firm and elevated.
• Redness and itching in the area of the bite.
b) Generals They occur due to an allergic reaction:
• Generalized itching.
• Inflammation of lips and tongue.
• Headache.
• General malaise.
• Stomach pain (colic type).
• Abundant sweating.
• Difficulty breathing
• Anxiety, being able to reach shock, coma and death.
- General attention. In all bites, the following should be done:
- Reassure the person.
- Provide rest.
- Remove the sting. Do it in the same direction you entered. Use the sharp edge of a knife or a plastic card for this.
- Apply compresses of cold water on the affected area to reduce inflammation and decrease pain and absorption of the poison. If you have suction equipment for poisonous animals (scorpion, spider, snake), vacuum several times.
- When an allergic reaction occurs, give an anti-allergic (antihistamine) and move the victim quickly.
Source
Bites.
They are wounds caused by the teeth of an animal or by man. They are characterized by being lacerated, avulsive or pungent; they present hemorrhages and sometimes shock. A person bitten runs a high risk of infection (including tetanus) because the mouth of the animals is full of bacteria.

Source
- Snake bites.
Snakes are gentle and not very aggressive animals; in general they flee from man. When they bite man they do so in self-defense and almost always in their natural environment, either because a person accidentally gets in their way or because they are bothered in some way.
However, snakes that live in captivity are responsible for a significant number of bites, and among their victims are veterinarians, biologists, zookeepers, collectors and trainers. The traces of the bite of a poisonous snake are characterized by the presence of small bleeding holes; the distance between the two fangs gives us the idea of the depth at which the poison is found; the depth changes according to the serpent.
The traces of the bite of a non-poisonous snake are characterized by a series of bleeding points in a row, parallel and superficial; there is no inflammation or pain. The manifestations and severity of the poisoning produced by snake bites depends on:
• Age and size of the victim.
• Previous health conditions.
• Species and size of the snake.
• Accidental bite of previously irritated animal.
• The states of the fangs and poisonous glands of snakes.
• Nature and site of the bite.
• Amount of poison inoculated.
• Duration in time between the accident and the appropriate care.
• Action of the poison.

Source
- General attention to bites.
Before starting first aid, it is necessary to identify the type of snake that caused the bite, as this helps in the treatment that will be provided at the healthcare center. Before a victim who was bitten by a poisonous snake, follow these steps:
- Place the victim at rest and reassure her. Suspend all activity, since the excitement accelerates the circulation, which increases the absorption of the poison.
- Remove the rings and all objects that may be squeezed by the affected part.
- If possible, wash the affected area with plenty of soap and water, without rubbing.
- Do not place ice, or make cross cuts on the bite marks.
- If you know that the victim will not receive specialized medical attention within 30 minutes, consider sucking the wound with the suction equipment for poisonous animals.
- This is not possible, perform punctures in the area of the bite with a sterile hypodermic needle. The depth varies according to the type of snake that caused the injury. Suction the liquid that you extract. Repeat this maneuver for the first 30 minutes after the bite. If not, apply the mouth suction on the marks by placing a plastic and suck through it for 30 minutes.
- Cover the injured area with gauze or dressings.
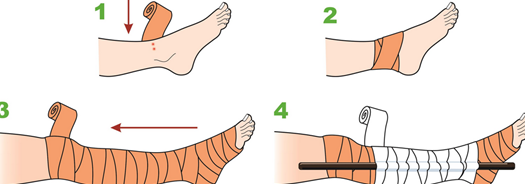
- Apply a wide and tight compressive bandage, but not excessively, from the hand to the shoulder or from the foot to the groin; the bandage must be tight enough to occlude superficial veins and lymphatic vessels, but it will never obstruct arterial circulation; this measure prevents the circulation of the poison and offers a time of safety, until medical attention is obtained. Do not let go In any case, the bandage should never be released until the antivenom serum has been administered and should be gradually loosened in the care center. If you do not have a bandage, it is helpful to immobilize the affected arm or leg with a splint or splint.
- In ophidic accidents due to corals or rattles, there is paralysis of the tongue and jaw, hyperextension of the neck, to open the respiratory tract.
- Be alert to prevent shock.
- Transport the victim to a healthcare center, for the administration of anti-venom serum and the management of complications.
Asphyxia.
Asphyxia is caused by the obstruction of the airways by some element. The first aid that must be applied includes the elimination of the elements that impede the passage of air to the lungs. Asphyxia is the inadequate supply of air to the lungs and oxygen to the blood. It is manifested by respiratory distress and purple discoloration of the skin and mucous membranes; It can cause respiratory arrest and death of injured.

Source
- Causes:
Among the causes of asphyxia are drowning, gas poisoning, overdose of narcotics, electrocution, obstruction of the airways by foreign bodies and strangulation.
- Symptoms of suffocation.
When a person is in the situation of suffocation, the first thing he does is grab his throat with his hand. That symptom should arouse our attention. The other danger signs are:
• The person loses the ability to speak
• Has a noisy breathing, in addition to breathing with difficulty and a weak cough
• Acquires a blue skin color
It is necessary to differentiate before applying first aid if the person is:
• An adult
• Child
• A pregnant woman
• Obese
When a person presents the first symptom of suffocation, grasping the throat with one or two hands, the first thing to do is:
Ask if you are drowning, if you can talk.
- If the victim is an adult:
- We will stand behind the person, who is drowning, with our arms around the waist.
- We will place our fist just above the navel and below the sternum, so that the thumb is against your abdomen.
- With the other hand, we will grasp the fist.
- Press up and in with a force that lifts the person who is choking off the ground.
- This action should be repeated as many times as necessary until the object that obstructs the respiratory tract has left or until the person loses consciousness. In that case:
- We will lay the victim on the ground.
- We will call the ambulance.
- We will start with cardio pulmonary resuscitation, as long as it is known to do.
- If we are able to see the object that obstructs the throat or trachea, we will try to remove it.
- If the victim is a child:
It is similar to what should be done to an adult.
- First, as in adults, we will stand behind the child and surround him with arms around the waist.
- We will close a fist with the thumb just above the navel of the child, and below the sternum.
- With the other fist, we will close our hands and press intermittently and quickly inwards and upwards.
- As in adults, until the child ejects the object or until he loses consciousness.
- In this case, we will also lay it down on the floor and call the ambulance, and if we know, we will start with cardio pulmonary resuscitation. In the same way as adults, if we are able to see the object that obstructs, we will remove it or try to remove it.
- If the victim is a pregnant woman or obese people:
- We will surround her with our arms at the level of the chest placing the fist in the middle of the sternum
- We will press firmly, backwards.
Fainting.
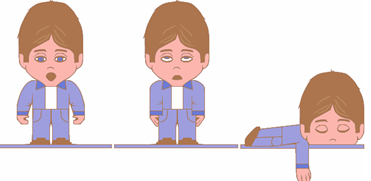
It is a state of sudden discomfort, with partial or total loss of knowledge, which lasts only a few minutes, this occurs when not enough blood reaches the brain for a short period of time. The causes of fainting or fainting can be:
• Strong emotions (fear, joy).
• Stale air in closed place.
• Long fasting.
• Pain.
Source
- Signs
• Sudden weakness.
• Paleness.
• Cold sweating.
• Blurry vision.
• Unconsciousness
• Sudden fall.
• Surface respiration.
• Weak pulse.
- Attention
- Place the victim in a place that has good ventilation.
- Loosen clothing to make breathing easier.
- Indicate that you breathe deeply, taking air through your nose and exhaling through your mouth.
- Ask him to cough several times. This stimulus improves the cerebral blood flow.
- If conscious, lie on your back, lift your legs to facilitate the return of blood to the brain.
- Do not give him anything to eat or drink.
- If the victim vomits, place it on its side.

Source
Fever.
It is the signal of different diseases, most of them infectious. The fever is a warning sign; it is the organic manifestation, which indicates the presence of disease and with its decrease the cessation or the improvement of it. In young children it is common for high fever to be accompanied by seizures. It is important to notice how it starts and when it is removed. This information can be useful to identify the disease. To know if a person has a fever, it is necessary to control the temperature.
Body temperature varies with the time of day. It is lower in the early morning hours and rises in the afternoon hours. It also varies according to the place where it is taken. The clinical thermometer or the touch assessment is used for its measurement. The normal temperature of the organism is 37 Degrees Celsius. In general, you should only lower the fever when the temperature is higher than 38.5 degrees Celsius.

Source
- Signals:
• Increased temperature to the touch, especially the neck and head, while the hands and feet are cold.
• Chill.
• Accelerated pulse and breathing.
• The patient spends bad night, especially in children who usually sleep well.
• Sudden loss of appetite.
• When the fever is very high, the patient may be irritable, sensitive to light, with a headache with restlessness or dizziness; Sometimes it can be accompanied by a state of mental confusion, called delirium, with disorientation in time and place, it can have hallucinations and convulsions.
• When a particularly active child stops moving, playing or being sleepy during the day.
- Attention:
- Bath with warm water for a period of 5 minutes; Do not dry, cover immediately with a light colored sheet or towel. Another method is to completely undress the child and aerate it throughout the body (using a newspaper or cardboard as a fan) for 15 to 20 minutes or until all the skin feels fresh, dressing it with clean, dry clothes, light and loose.
- Initiate hydration with oral serum, water or other due.
- Break the food without forcing its consumption.
- Administer an anti-rheumatic medication (aspirin or dolex) taking into account the precautions.
- Keep the place cool and ventilated.
- Check the temperature every 6 hours.
- Consult the doctor to discover and treat the cause.
- Disinfect the thermometer with soap and alcohol water.
- Shake it until it reaches minus 34 degrees Celsius.
- Place the thermometer under your tongue; Leave it on for 3 minutes. In the armpit; Leave it on for 5 minutes.
- If it is a child, check the temperature of the armpit by holding the arm flexed and close to the chest. Do not leave it alone.
- Perform the reading by placing the thermometer at eye level with the colored band on the opposite side and look for a silver strip that comes out from the ampoule and ends at the point that marks the temperature.
- The divisions of the thermometer are called degrees. The divisions between grade and degree are called tenths and allow accurate reading.
- Then wash and disinfected with alcohol.
Thank you for reading.
For more information, visit the following links:
This post has received a 0.59 % upvote from @buildawhale thanks to: @theborges. Send at least 1 SBD to @buildawhale with a post link in the memo field for a portion of the next vote.
To support our daily curation initiative, please vote on my owner, @themarkymark, as a Steem Witness
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
This post has received gratitude of 0.54 % from @appreciator thanks to: @theborges.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit