This is my first science-related post, and I’m pretty excited about this, because it’s an opportunity for me to expand my scope of knowledge. I studied Microbiology in the University, though after school, I got trained as an ophthalmic technician. I find a need to brief my readers on the different eye diseases which can be preventable, if the right things are done.
I'm starting a series on the different eyes diseases caused by Diabetes mellitus, today, I will write on diabetic retinopathy (DR).
Diabetic patients cannot escape this condition, at some point in their life it will show up, that’s why the American Optometric Association advised every diabetic patient to have a comprehensive dilated eye examination once a year. Vision loss will be reduced if early diagnosis and treatment is done.
WHAT IS DIABETES?
According to International Diabetes (IDF) Diabetes Atlas 2017;
Diabetes mellitus, more simply called diabetes, is defined as a chronic condition that occurs when there are raised levels of glucose in the blood because the body cannot produce any or enough of the hormone insulin or use insulin effectively. Insulin is an essential hormone produced in the pancreas gland of the body, and it transports glucose from the bloodstream into the body’s cells where the glucose is converted into energy. The lack of insulin or the inability of the cells to respond to insulin leads to high levels of blood glucose, or hyperglycaemia, which is the hallmark of diabetes. Hyperglycaemia, if left unchecked over the long term, can cause damage to various body organs, leading to the development of disabling and life-threatening health complications such as cardiovascular disease, neuropathy, nephropathy and eye disease.
From the definition of diabetes above we can easily identify the different types of Diabetes mellitus which are Type 1 diabetes, Type 2 diabetes and the gestational diabetes.
TYPE 1 DIABETES (T1D)
This occurs when our body’s immune system mistakenly destroys the cells that produce insulin in the pancreas. Though a cause of this attack is not fully understood, scientist initiated that it may be due to genetic or environmental factors. It is mostly found in children, though it can be diagnosed at any age. Presently, there’s no cure, and it also not preventable too, but there’s no cause for alarm, because with proper daily insulin injections, maintaining a healthy diet and lifestyle, and regular exercise, any complication from T1D can be reduced and avoided.
TYPE 2 DIABETES (T2D)
T2D happens when the cells are not able to respond to the insulin produced by the pancreas, leading to what is referred to as insulin resistance. The pancreas is stirred up to produce more insulin to balance up the demand for insulin, at a long range, the supply of insulin will definitely reduce, because the pancreas will become weak to meet the demand. T2D is responsible for mostly all cases of diabetes, according to IDF Diabetes Atlas 2017, its account for around 90% cases of diabetes mellitus. It is always confused with Type 1 diabetes because they have similar symptoms, like frequent urination (polyuria), reoccurring hunger (polyphagia), dry mouth and abnormal thirst. T2D seems to show up very late, so the early signs found in T1D are not present here.
GESTATIONAL DIABETES (GDM)
Gestational diabetes mellitus (GDM) or simply hyperglycaemia in pregnancy is a type of diabetes that occurs during pregnancy. GDM occurs when there’s a little increase in the sugar level, but when there’s a major rise in the sugar level it’s called Hyperglycaemia in pregnancy. Women who develop or have gestational diabetes mellitus are at risk of developing severe diabetic retinopathy.
There are also less common types like monogenic and secondary diabetes. Monogenic diabetes is due to mutations (a change in a single gene); neonatal diabetes mellitus (NDM) and maturity-onset diabetes of the young (MODY) are the two main example of monogenic diabetes.
Secondary diabetes is formed as a result of other predisposing factors like a disease or an injury to the pancreas, medications or other medical conditions like Cushing’s Syndrome.
If you notice these symptoms such as abnormal taste, constant hunger, frequent urination, dry mouth, weight loss, fatigue, wounds or small cuts that do not heal, tingling and numbness in your hands and feets, in an individual or even your own self, quickly get to the hospital and get diagnose, because these are early signs of diabetes.
Diabetes if left undiagnosed or unmanaged for longer period of time can lead to complications which are mostly irreversible, but if detect early can be curbed and controlled. Eye diseases mostly caused by increased level of glucose in the blood are glaucoma, cataract, diabetic retinopathy (DR), and diabetic macula edema (DME).
DIABETIC RETINOPATHY (DR)
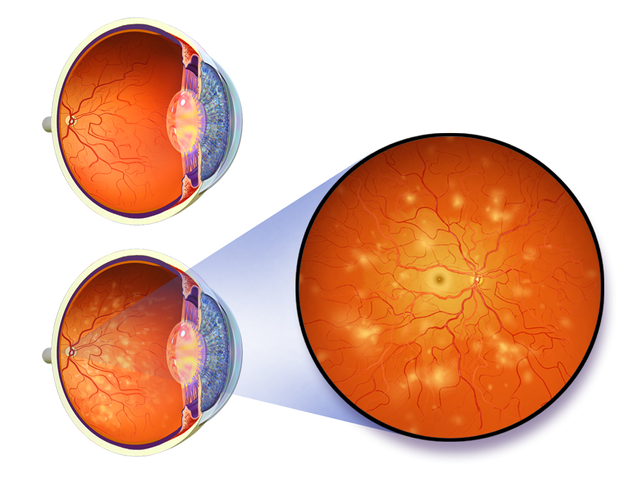
This is a complication of diabetes mellitus caused by damages to blood vessels that supply blood to the retina. The retina is the part of the eye that receives light rays focused on the lens, converts it to signals and sends it to the brain, which are then interpreted as images.
DR occurs when long periods of high blood sugar causes the lining of the blood vessels in the eye to thicken and develop leaks or bleeds (hemorrhage), this causes the retinal tissues to swell causing blurred visions. In an advanced stage, due to poor circulation from the leaks, new fragile cells are formed on the surface of the retina, leading to more leakages and retinal detachment (this occurs when the retina is detached from the normal position due to scar cells from the leaked vessels).
Wikimedia Commons author by National Eye Institute, National Institutes of Health (Public Domain): Slit lamp photograph showing retinal detachment.
STAGES OF DIABETIC RETINOPATHY
There are two stages of diabetic retinopathy; **Nonproliferative diabetic retinopathy** (NPDR) and **proliferative diabetic retinopathy** (PDR). But NPDR is further broken down to ***mild***, ***moderate*** and ***severe*** NPDR as the disease progresses. • Mild nonproliferatve diabetic retinopathy always starts with tiny bulges called microaneurysms forming on the blood vessels. This may lead to the blood vessels leaking fluids or blood into the retina.• In moderate nonproliferative diabetic retinopathy, the blood vessels rupture losing their abilities to supply blood and fluid to the retina. Blurred vision can be noticed here, since this might lead to swollen macula; the part of the eye responsible for central vision.
• Severe nonproliferative diabetic retinopathy occurs when part of the retina (deprived of blood supply due to the ruptured blood vessels) secretes growth factors which trigger the retina to grow new blood vessels.
• Proliferative diabetic retinopathy is the advanced stage of diabetic retinopathy. Here, new fragile blood vessels are formed on the surface of the retina and grow into the vitreous. Since these new blood vessels are fragile, they may likely bleed and leaks fluids again into the retina. This may lead to retinal detachment and vision loss if not treated.
SYMPTOMS
The early stage of Diabetic retinopathy always goes unnoticed until its get to the advanced stage where there is an appearance of “floating” spots caused by bleeding from the new fragile cells formed. Other common symptoms are fluctuating vision, Impaired color vision, dark or empty areas in your vision.

Wikimedia Commons Author By National Eye Institute, National Institutes of Health (Public domain): Normal vision
DIAGNOSIS

[Image of a Non-mydriatic retinal camera used to take images of the Retina]
Comprehensive eye test to check for diabetic retinopathy always start with a Visual acuity test; to check for the ability of the patient to see from different distances. Then Tonometry test is done to measure the pressure in the eye, and an optical coherence tomography (OCT) is performed to get a detailed images within the retina. Pictures of the retina could be taken without dilation of the eye using a non-mydriatic retinal camera; its takes the picture of the fundus; which consists of the retina, macula, optic disc, and fovea.
If proliferative diabetic retinopathy is suspected, detailed images of the retina will be capture through a technique known as fluorescein angiogram to search for leaked or damaged blood vessels. Here, a special dye fluorescein is injected into the arm vein, and pictures of the retinal blood vessels are taken immediately the dye get to the eye.
TREATMENT

Flickr image author by National Eye Institute, National Institute of Health: Laser Surgery to Correct Leaking Blood Vessels
Anti-VEGF injection therapy is the first-line of treatment for diabetic retinopathy patients. Here, anti-VEGF drugs are injected into the vitreous of the eye to block the growth factor; vascular endothelial growth factor, which causes blood vessels to grow and leak fluids into the retina.
A procedure called laser coagulation will be done if new blood vessels are already formed. This involves focusing a laser light beam in areas of the retina away from the macula. This laser burn stops the formation of new blood vessels and shrinks any blood vessels that were formed. This procedure is also used to seal any leaking blood vessel.
A procedure called Vitrectomy can also be done if the fluids are already leaking into the vitreous causing vision loss. Here, a little hole is created in the eye, and all the liquid in the vitreous is drained and replace with a salt solution. The patient will be able to go home that day but will have to wear a patch to protect the eye, and eye drops will be applied against infections.
CONCLUSION
All this can be avoided if diabetic retinopathy is diagnosed early through regular (annually) examination of the retina, starting from when diabetes was first diagnosed. Keeping blood glucose and pressure levels near normal as possible can also help in delaying diabetic retinopathy from progressing to the proliferative stage. Also avoiding alcohol, hard drugs and smoking is advisable. Taking your prescribed medication, sticking to your diet by the dietician, and exercising regularly will do more help in reducing the progress of the condition.
REFERENCES
If you write STEM (Science, Technology, Engineering, and Mathematics) related posts, consider joining #steemSTEM on steemit chat or discord here. If you are from Nigeria, you may want to include the #stemng tag in your post. You can visit this blog by @stemng for more details. You can also check this blog post by @steemstem here and this guidelines here for help on how to be a member of @steemstem. Please also check this blog post from @steemstem on proper use of images devoid of copyright issues here.

)
)
)
Being A SteemStem Member
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Wow
Great content,thanks
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
It was made just for you.
Go ahead and get the world informed about diabetes mellitus a save a soul.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Wow nice post@yanga.. The world need to hear and see this... You have just gpt me informed... I have been having a diff mindset towards diabetes, but u just woke me up now. Thanks alot.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit