Moving my old engineer.diet blog posts to steemit. I've moved all my blogs to steemit so I'm dismantling my paid-for WordPress hosting. This post is an old one from march 29th 2016 that I thought was worth salvaging.
From shady Statin research to poor dietary guidelines.
In this post I will look a bit deeper into how shady science , in a very unfortunate way ,found itself a foundational place in nutritional science, and how this science has managed to, even today poison dietary guidelines and in effect poison the health of whole populations.
I will look at this from the perspective of the Dutch dietary guidelines, but judging from many other national nutritional guidelines, a similar cascade has probably been applied in the creation of other such national guidelines. So let’s look at the dutch Disk of Five (Schijf Van Vijf) and trace how the advice came to be.
The new Dutch dietary guidelines refer to saturated fats quite often and once to LDL-cholesterol. These are foods the guidelines wants us to avoid, and the foods we should use instead:
- Coffee high in cafestol; use filtered coffee instead.
- Hard margarine; use soft margarine instead
- Hard baking fats; use liquid margarine or olive oil instead.
- Hard deep-frying fats; use vegetable oils instead
- Butter; use soft margarine instead for bread or liquid margarine for baking.
- Coconut oil; use vegetable oils or olive oil instead.
- Non-lean meat cuts; use lean cuts instead.
- Full-fat dairy; use low-fat dairy instead
- Croissants; use full-grain bread-buns instead.
- Cookies; use full-grain peanut-butter sandwich instead.
- Chocolate; use fruit and nuts instead
Next to these, the guidelines advise the consumption of legumes for its LDL lowering properties.
There are issues with many of these guidelines, issues we will get to later in this article. First we will look at why the the Dutch Nutrition Center made these recommendations. What reasoning was behind them and where did the data for this reasoning originate? Well this is where things get a bit complex. The Dutch Nutrition Center claims their recommendations are science based, and objectively speaking they are. So how did things go so wrong anyway? Let’s have a look. The guidelines by the Dutch Nutrition Center are themselves based mostly on a more abstract guideline by the Dutch Board of Health (Gezondheidsraad). These guidelines come with multiple background documents, including one on macronutrients, that I tried to give feedback on when it was published due to in my view questionable use of LDL-c as causal marker and control for cardiovascular disease. My input was rejected as the Board of Health claimed the subject was covered in another document describing the use of a set of three markers:
- Blood pressure
- LDL-cholesterol
- Body Mass Index
We will leave blood pressure for what it is, and for BMI I’ll refer to my earlier posts on that subject. The thing we are interested in here is LDL-cholesterol. The document justifies its use of LDL-cholesterol as stand-in for CVD endpoints by refering to a publication by the American Institute of Medicine (IOM) entitled Evaluation of biomarkers and surrogate endpoints in chronic disease.
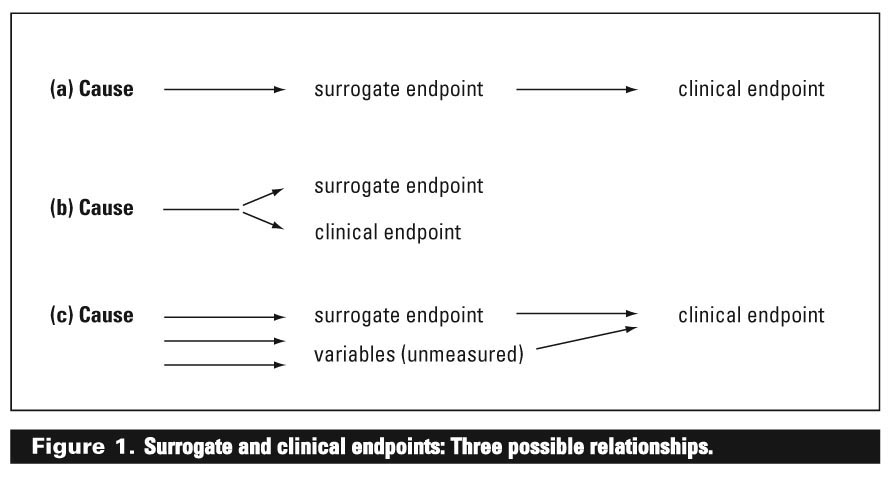
And this is where the real problem starts. Surrogate endpoints. Remember that correlations aren’t necessarily the same as causation. Remember the difference between a good risk marker and a usable control? Well, this document, to some extent, for the Dutch Board of Health apparently to a decisive extend claims that LDL-c can be treated as being causal, that is, LDL-c can be used not only as a risk MARKER, but actually as a control. We won’t go into LDL-c as risk marker here. The case of LDL-c being a risk marker is solid. There are clear signs that there are multiple much better markers available today, in fact the same goes for the other two markers we just mentioned, but let’s accept LDL-c as a useful marker. The interesting part is: how does the document make the leap from marker to control, or as the document refers to it, surrogate endpoint?
The answer is: intervention studies. Statin based intervention studies to be precise. So to summarize, the current dietary advice hinges on a collection of statin intervention trials. On first glance there wouldn’t seem to be anything wrong with that. We have intervention trials where lowering bad cholesterol (LDL-c) has shown statistically significant reduction of real CVD linked endpoints, so LDL-c is indeed a useful control, right? Well not quite. It could be if lowering cholesterol was all that statins do, and it would be if next to being statistically significant, the results also had practical significance. And guess what, on both accounts this turns out not to be the case. First, statins combine a whole set of potentially CVD preventative related properties:
- Lowering LDL-C
- Thinning the blood
- Acting as antioxidant
- Acting as anti-inflammatory agents.
- Lowering triglyceride levels
And on the other side of the spectrum, statins have actually been linked to CVD causing effects. In fact, some recent trials actual show increased CVD in statin treated groups.
- Worsening cholesterol sub-group/size profiles
- Reduce protection from artery calcification by inhibiting K2 synthesis.
- Reduce protection from peroxidative stress by impairing selenium containing proteins.
- Impair muscle (including heart) functions through depletion of coenzyme Q10
So far we only looked at CVD related properties, but statins are not without side effects:
- Vitamin D depletion
- Severe cognitive issues including memory loss
- Increased risk of diabetes
- Severe muscle problems
- Liver damage
- Birth defects
- Erectile problems
Some of these side effects come with their own increased mortality numbers. Others just diminish the quality of life without actually killing you. Recent research has shown that using statins for many many years will increase your life expectancy by just a few days. Not that impressive considering that the price for those days may be years of muscle, cognitive and erectile problems. And then there is the controversy surrounding statin trials. The most notable being the JUPITER trail. But also recent meta analysis that show that statin results have been exaggerated and side effects have been downplayed in a scaringly structural way. Multiple MDs as a result of the controversy have called for a complete reappraisal of the cholesterol theory of heart disease. The bottom line: Statin trials, from a data engineering perspective could never prove LDL-c causality for CVD, and could never prove the suitability of dietary changes aimed at LDL-c reduction as an in any way useful control for CVD.
So let’s look again at some of the guidelines that these statin trials ended up spawning. Remember that two known positive effects of statins were its function as antioxidant and anti inflammatory agent? Well, let’s look at how the Dutch dietary guidelines are doing on those. Especially those guidelines based on the LDL-c hypothesis. The first thing that stands out is the use of cold fat sources high in polyunsaturated omega 6 fats as alternative to fat sources high in saturated fats. It is well established that an imbalance of omega 6 and omega 3 intake works pro-inflammatory. As such, saturated fats, while leading to higher LDL-c levels than omega-6 fatty acids, also lead to lower inflammation when compared to omega 6. Inflammation has not only been linked to CVD, but to a multitude of major diseases including diabetes and cancer.
Than there is the advice for cooking fats. Unsaturated fats can be healthy in the right proportions. At a proper ratio of omega 6 to omega 3, unheated polyunsaturated fats can undisputedly be healthier than saturated fats and so can monounsaturated fats. But that is cold. Once you start cooking with it, the tables turn. While LDL-c as shown above is highly questionable when used as control, the link with ‘oxidized’ lipoproteins is significantly more convincing. Oxidized unsaturated fatty acid consumption is linked quite strongly with oxidized lipoproteins. So where there is sense in replacing butter with MUFA-rich oils for cold unheated usage, when it comes to cooking, the reverse must be considered. Saturated fats in butter and coconut oil are stable fats that don’t oxidise as quickly as unsaturated fats in olive oil and vegetable oil. Suggesting the use of MUFA and PUFU over SFA for cooking purposes should be considered the most questionable advice in the dietary guidelines.
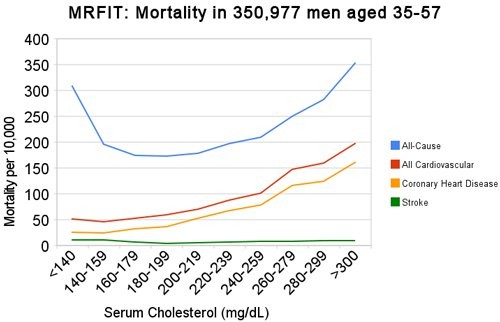
Finally there is the epidemiological data. High cholesterol isn’t the only cholesterol related risk marker that we can identify in the data. Low cholesterol is also a serious risk marker. Thus a population wide guideline with the effect of the reduction of cholesterol levels may very well backfire. Looking at the China Study II data set, SFA intake overall is relatively low. When however we at mortality figures and look at the top ten correlation for foods that potentially improve the probability to live to the ripe old age of 80 years old, SFA (and MUFA) truly stand out. When we look at cholesterol levels, the lowest levels are linked quite strongly to the highest mortality. Unfortunately, due to distribution concerns we can’t check the link for statistical significance, but we can take it as a strong indication that cholesterol lowering might be detrimental to the health of certain groups of people within the population.

Summarizing, statin trials, due to the complex working of statins, the controversy surrounding some statin studies, the at-best unimpressive effects of statin intervention, and the combination of different beneficial and decremental effects of its use, must be seen as being inconclusive with regards to LDL-c being causal for CVD. If we combine this fact with known health effects of some of the SFA replacements that are advocated in the guidelines, we can only conclude that shady statin trials poison not only nutritional science, but in effect literally poison the whole population of countries that indirectly base their dietary guidelines on the outcomes of these statin trials under the mistaken assumption that the results of these trails are in any way conclusive with respect to the causality of LDL-c for cardiovascular disease.
What do you think about the Ketogenic philosophy?
It is best explained in Youtube channels such as "What I've Learned" and Eric Berg (but beware of his and his peers' claims about honey, which in reality is worse than white sugar)
They concentrate about the dietetic part of this philosophy, but I guess there is more to it, like minimizing light in order to reduce cortisol release.
I do recommend listening to most of what they say, while applying some consideration/discretion.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit