Greetings Friends Steemians,
Today is a pleasure to present a topic that brings a lot of discussion in the medical journals of traumatology, not only because of the diversity of information that can be found through this subject so studied, but it is our daily bread in the room Emergency of a hospital in the area of traumatology.
Wanting to be a traumatologist was not an idea that came to me overnight, since I stepped into the hospital during medical school I was looking to enter the traumatology area. I had always had the great curiosity to know how the fractures of the children healed, it was always something so fast, and in the end they ended up happy with a cast. Until I was too lucky to see when a broken wrist came along.

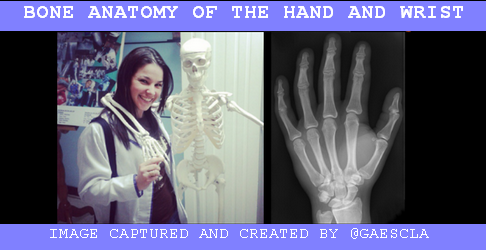
NOTIONS OF ANATOMY OF WRIST.
The wrist is the part of the upper limb that is going to join the hand with the forearm, and this will be joined by bones and tendons; It is important to know the bones that the wrist brings and how it articulates with the bones of the forearm.
If we see the bony part of the hand is much more illustrative for all of us: we have the fingers of the hand that are made up of 3 phalanges with the exception of the thumb that only has 2 phalanges, these at the same time are joined with the bones that are they find in the palm of the hand: called metatarsals, and if we go more proximally we arrive at the wrist that is conformed by 8 huesillos that together are denominated like the carpus; In a cross section of the wrist, these are arranged in 2 rows with 4 bones: each of them has names: we must always name them in a coordinated order, for example from lateral to medial, the most proximal row that articulates with the bones of the forearm are: scaphoid (NAVICULAR), semilular (LUNATE), pyramidal (TRIQUETAL), pisiform. The second row more distal and articulates with the metatasianos are: Trapeze (TRAPEZIUM), trapezoid (TRAPEZOID), big bone (CAPITATE) and hamate
The forearm is well known for having 2 bones in it: the radius and the ulna, in Spanish it is also known as cubito.
The bone of the forearm that is going to join with the wrist, exactly with the first row of the most proximal carpus, is the radius.
Here I present to you my friend Felito, he has always been happy and willing to teach us everything about him:
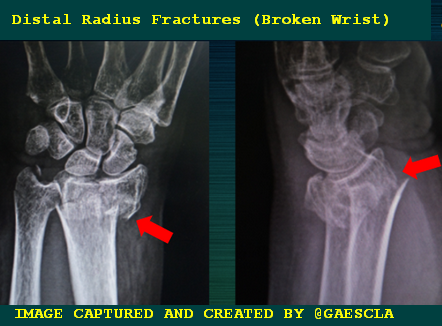
BROKEN WRIST or WRIST FRACTURE
When we refer to fractures of the wrist, the most frequent are those that occur at the distal end of the radius. For this I want to present a real life clinical case.
In theory and in practice it is important to have extensive knowledge of anatomy to be able to classify a fracture in order to define its prognosis and treatment.
Arriving at the Emergency
Getting to the emergency is always a chaotic moment, but as we are taught in medical school and in any rescue course the main thing is to keep calm, although we doctors always start all our cases with what we call History of presentation of a complaint or History of the current illness, which are the details of the chief complaint ... we really do this at the end of having all the data and we sit down to write it with more calmly.
Complaint History Patient: 72-year-old female who according to the beginning of the history of the current illness on 02/07/18 after falling from her own feet, with upper right limb in extension and wrist in dorsiflexion, presenting pain, edema, bone crackle deformity in the right wrist with limitation for its function, go to a medical care center where an indicative and imaging clinic is evaluated, presenting a distal 1/3 fracture of the right radius.
CHECKING THE X RAYS
Here we can see a clear example that seeing 2 projections is very important, where in the anteroposterior view there is no fracture but in the lateral view yes. (X-rays of the left leg). Law of life we must always be very observant, but not only see one side, many can be a surprise.
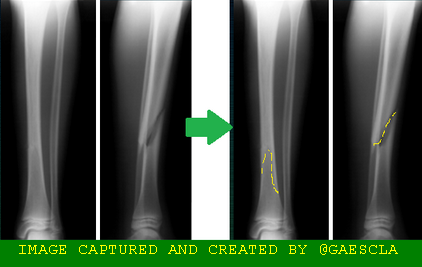
For any bone deformity, the RX study is the study of choice and should always be done before manipulating any fracture. Although the clinic always prevails in the case of fractures, it is always important to document. One of the gold rules of radiology is to make projections an articulation above and an articulation below the deformity: IMPORTANT FACT.
Studying MORE Our Patient
For everything there is time, we must always be calm in any medical situation, and highlight our detective skills so that all the decisions we make with our patient are correct. After knowing the current illness of our patient, and having the diagnosis in front of our eyes, we must focus on the antecedents of our patient:
Past medical history:
Denies allergy to medications and basic pathologies, refers 2 apparently healthy children, living parents apparently healthy. Occupation: teacher of mathematics. Dominant hand: right.
EXPLAIN DIAGNOSTICS: MEDICAL CHALLENGE
I consider that in traumatic situations patients lose their sense of hearing, they increase their sense of sight and their ability to speak, so explaining a procedure is like an art: you have to have a lot of patience and having x-rays can better illustrate everything to be done.
We present a stretcher, where we send them to go to bed, it is indicated that you should place your arm inside a girth, once positioned our patient, it is explained that it must be pulled or carried to the site, we give the patient the option to place anesthetic local in the focus of the fracture.

HEALING FRACTURES
We doctors must always have everything at hand, because once the reduction is made we can not lose it, depending on a series of criteria and many parameters, we decide where and how to perform the reduction maneuver. For this we have our dear plaster room, which will depend on the hospital where we work, here I present where we made this case of our patient. It is an office that is modified every time a patient arrives to pull.

MATERIALS or EQUIPMENT
✅Fixed stretcher: It is a stretcher that does not have wheels, because if we are going to pull, we do not want the table to move. If in Spanish there are many ways to name things, to the stretcher when the patient is in it or when we talk about performing a procedure in the we say table.
✅Cinch: This is a padded ring that is hung from a fixed tube in the traction area, in which the affected upper limb is placed to make axial traction easier.
✅ Injector, sterile gloves, local anesthetic, alcohol.
✅6 bandages of mineral gypsum
✅Wadding.
✅Gypsum cart where the water goes in a basin
✅ X-ray viewer and the RX with 2 PROJECTIONS.
✅ 2 trained assistants: they can be doctors or studying the specialty of traumatology
✅A traumatologist 😉👍
PROCEDURE DESCRIPTION
We continue with our special case: Mrs. A. Fractured. PLAN: Closed reduction of fracture plus brachypalpal cast plastering.
It is always important to start our procedures with "Previous standards of asepsis and antisepsis": it is only the cleaning of the fractured area and of course absolute alcohol with a gauze from the center to the periphery in a centrifugal form, local anesthetic is placed in the focus of the fracture where it is extremely important to know the anatomy, proceed to perform longitudinal traction maintained, reverse play the mechanism of production of the fracture after evaluation of radiological study, maintain axial traction, place bandages of cotton (padding) protecting the areas of pressure, make a brachiopapial cast in 2 beats, that is, being careful not to apply pressure, slip a bandage with the correct limits, remove the upper part of the cinch, keep the elbow with 90 ° of flexion and hand to the zenit, perform radiological control study, evaluate satisfactory reduction and in the second time complete a brachylatedpalm cast .
Video
TIME OF PRAISE
After the cast, and the patient feels that everything is fine, all the emotional relatives even applaud the doctor as a hero, it is not a lie, literally like a hero, not only for our performance and all the years of study, but also for our courage in performing procedures such as these as Cruel as they call it, and more if the reduction is made by a doctor as cute and tiny as the one described in this post.
PERSONALIZED MEDICAL INDICATIONS
We as doctors know that there are dangers or complications of the posterior stabilization of a fracture with a cast, normally it is not necessary to indicate oral analgesics after this, it is to emphasize that the treatment to cure your broken bone is the cast, and remain clean and dry, in addition to keep the arm in a position of decline can cause edema that can cause decreased circulation, called compartmental syndrome, which can bring many severe sequels, so after all happened patients feel a lot fear, once having this warning, they want to stay hospitalized.
Once again our face changes and we explain the ways in which they can avoid the occurrence of the dangers or complications, and for that reason they must go to the 72 hours to be evaluated again by the doctor who indicated the treatment, All this delivered to the patient by written, and leave it reflected in the emergency notebook.
Always highlighting your indications, it does not matter that you repeat it many times and pass it in writing, repeat it to the patient and all those who will help this person during their medical rest:
** _ Never Forget: KEEP ARM ON HIGH, MOVE FINGERS, DO NOT PAINT NAILS, DO NOT SCRATCH, DO NOT WET, OR PAINT THE CAST, GO TO 72 HOURS WITH THE DOCTOR ._ **
CONCLUSIONS
Bibliographic reference
Terry Canale S: Campbell Cirugía Ortopédica-10ª edición-2004-Elsevier— España
Rocwood & Greenn: Fracturas en el adulto. 2003 Reimpresión 2007. Editorial Marban.

Story and original support material of @gaescla


Business card designed by @romulexx

Collage Edited in paint with own images of @gaescla permanent and dynamic assistance to all the academic activities where Science lives
Muy explícito. Genial Gaby!
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
Gracias @gatoconbotas saludos!
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
good post! thanks!
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit
hi @donrito thanks so much.
Downvoting a post can decrease pending rewards and make it less visible. Common reasons:
Submit